All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
IMWG recommendations for infections in multiple myeloma
Infection is a major concern in patients with multiple myeloma (MM), leading to morbidity and mortality, and it may occur due to several reasons. Infection risk is highest within the first 3 months of diagnosis and during treatment for MM and it may peak again in cases of relapse and severely impaired immunity. Preventive measures play an important role in reducing the risk; however, there are no global guidelines in this regard.1
Recently, Noopur S. Raje et al.1 on behalf of the International Myeloma Working Group (IMWG) published consensus guidelines and recommendations based on available evidence about infection risk and prevention in MM, including individualized strategies from a panel of 36 experts gathered by the International Myeloma Society.1 Here, we summarize these recommendations for preventing and managing infections in patients with MM.
Infection risk and prevention
Patients with newly diagnosed MM are at high risk for infection, which may lead to premature death, even before induction therapy. Some patients are at greater risk for early and severe infection, including those with:
- high tumour burden (International Staging System II–III),
- markedly high concentrations of serum lactic dehydrogenase,
- poor performance status, and
- impaired renal function.
Newly diagnosed patients should be vaccinated against Streptococcus pneumoniae as early as possible and given a broad-spectrum antibacterial agent. The management of infections should be individualized based on infection risk (Figure 1).
Figure 1. Risk-adapted antimicrobial prophylaxis*
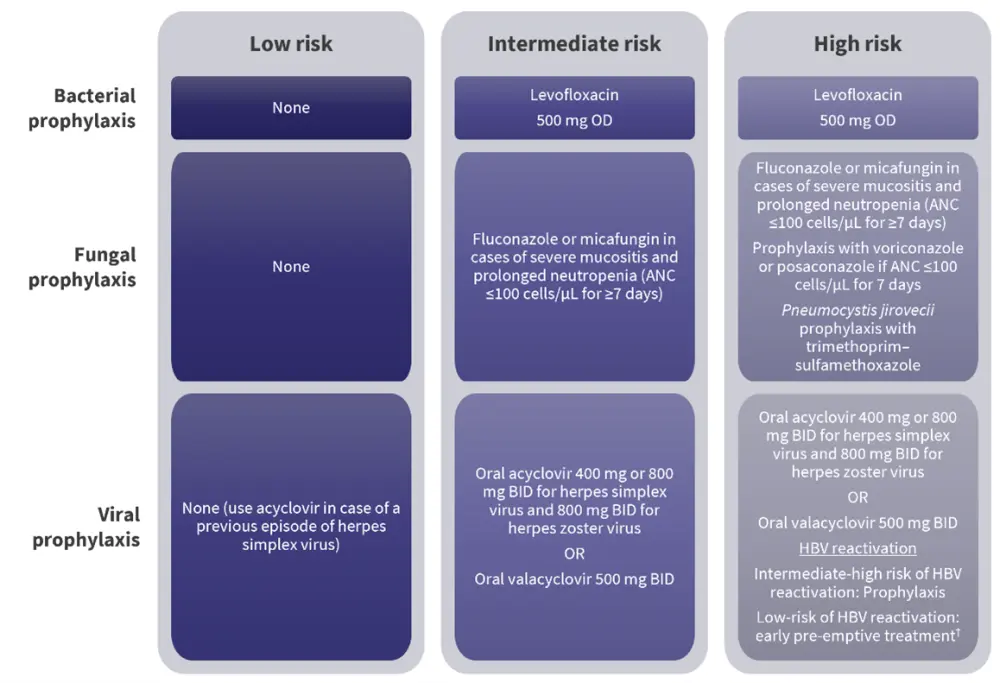
ANC, absolute neutrophil count; BID, twice daily; HBV, hepatitis B virus; OD, once daily.
*Adapted from Raje, et al.1
†For treatment and pre-emptive strategy, consider tenofovir (in case of previous exposure with lamivudine) or entecavir.
Infections may occur due to several factors related to disease, treatment, or the individual patient. Figure 2 and Figure 3 summarizes disease- and treatment-related factors (respectively), possible infectious events, pathogenesis, and preventive measures.
Figure 2. Disease-related factors for infection*
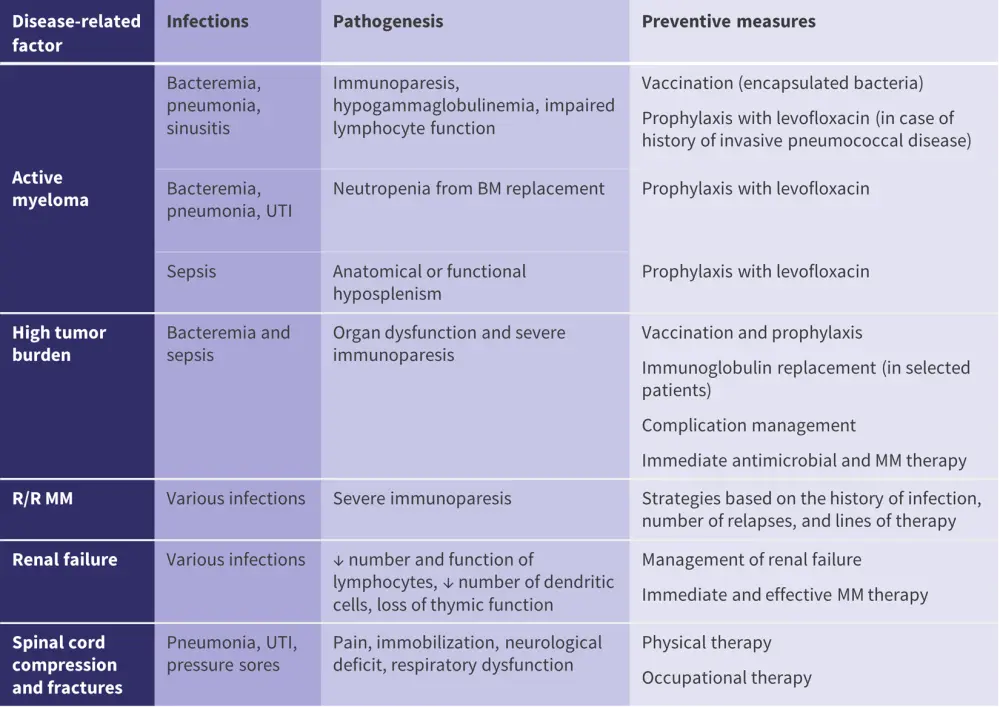
BM, bone marrow; MM, multiple myeloma; R/R, relapsed or refractory; UTI, urinary tract infection.
*Adapted from Raje, et al.1
Figure 3. Treatment-related factors for infection*
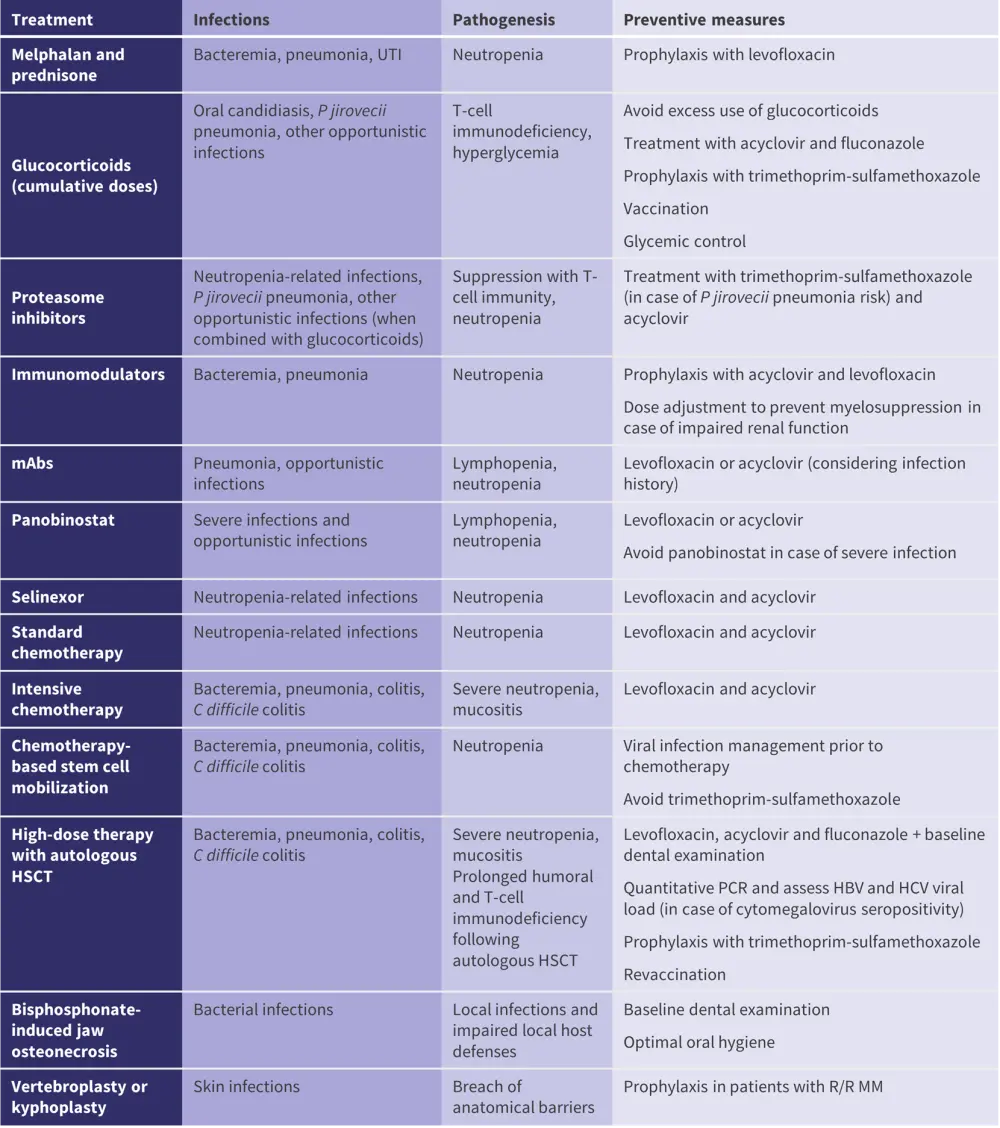
HSCT, hematopoietic stem cell transplantation; mAbs, monoclonal antibodies; MM, multiple myeloma; R/R, relapsed or refractory; UTI, urinary tract infection.
*Adapted from Raje, et al.1
Age of 75 years or older, frailty, poor performance status, or comorbidities have been associated with increased risk of shingles, pneumonia, and urosepsis due to immune senescence and deficiency related to impaired renal and liver function. In these patients, risk-adapted MM therapy and prophylaxis with acyclovir should be considered.
Patients with previous infection history are at risk for viral and fungal infections, Clostridium difficile colitis, and opportunistic infections, and it is important to consider history of infection and immunization as well as targeted prophylaxis. For Staphylococcus aureus colonization-related infections, decolonization-targeted therapy should be considered. In case of exposure to water and food-borne pathogens, pneumococcal vaccination should be considered, and patients should be informed.
Vaccination
Recommendations on vaccines are similar to those published by the European Myeloma Network in 2021 in terms of vaccine type and timing. The differences/additions in the IMWG report include:
- Only inactivated vaccines are recommended in patients with MM due to the lack of safety/efficacy data about live vaccines.
- Lenalidomide monotherapy has been associated with improved response to vaccination (no concurrent use of dexamethasone).
- Prophylaxis with varicella zoster vaccine is recommended to continue where indicated, irrespective of vaccination status.
- Passive immunization is recommended in patients with MM in case of exposure to individuals with hepatitis A, varicella, or measles.
Other recommendations
- Intravenous immunoglobulin should be used in particular cases, such as life-threatening infections and an immunoglobulin concentration <400 mg/dL with recurrent infections.
- In afebrile patients, prophylaxis with granulocyte colony-stimulating factor is recommended.
- In case of exposure to varicella, herpes zoster, and hepatitis A in immunosuppressed patients, immunoglobulin prophylaxis may be beneficial.
- Patients and caregivers should be informed about the regional risks, disease transmission patterns, and outbreaks. Additional recommendations may include avoiding raw food and uncooked meat, close contact with patients with tuberculosis, or activities that may increase the risk of fungal infections. In case of traveling to endemic areas of infection, consultation with an expert before traveling, as well as travel vaccines and prophylaxis with antimicrobials are recommended.
Conclusion
This report highlights the importance of an individualized strategy to prevent infections in patients with MM, which may be useful for treating physicians. Some patients are at greater risk of early and severe infection, which leads to early death; these patients should be considered for prompt preventive measures to manage infections.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?

