All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Novel risk score for predicting early relapse in patients with multiple myeloma
Do you know... Which of the following possible factors that were analyzed to develop a new early relapse prediction score for multiple myeloma patients following transplantation were included in the final model?
Early relapse following autologous hematopoietic stem cell transplant (auto-HSCT) is associated with a poor prognosis, as are high-risk cytogenetic features and failure to achieve a complete response.1 Previously, the Center for International Blood and Marrow Transplant Research (CIBMTR) and GIMEMA groups have created methods for predicting which patients are at risk of early relapse, which take into account factors such as bone marrow plasma cell content, cytogenetic risk, and albumin levels. Both of these methods split patients between high-, intermediate-, and low-risk scores, and overall survival and progression-free survival (PFS) were the endpoints. However, the PFS of each category wasn’t readily distinguishable immediately following auto-HSCT.1
During the 48th Annual Meeting of the European Society for Blood and Marrow Transplantation (EBMT), Beksac1 discussed taking this further to develop a scoring system to predict early relapse following auto-HSCT for patients with multiple myeloma (MM) in the EBMT database who were treated with 200 mg/m2 melphalan (Mel200) or 140 mg/m2 melphalan (Mel140).
Study design
From the EBMT database, 14,367 patients who had undergone auto-HSCT were selected and separated into a training cohort and a testing cohort.
The training cohort, also called cohort 1, consisted of 7,228 patients who underwent auto-HSCT between 2014 and 2017 and were conditioned with Mel200.
Possible factors analyzed for the prognostic model included the following:
- Age
- Sex
- International Staging System (ISS)
- Disease status
- Karnofsky score at auto-HSCT
- Duration between time of diagnosis and auto-HSCT
The testing cohort was divided into two external validation sets:
- Cohort 2: Patients transplanted and treated with Mel200 between 2018 and 2019 (n = 5,616)
- Cohort 3: Patients transplanted and treated with Mel140 between 2014 and 2019 (n = 1,523)
Results
The characteristics of cohorts 1 and 2 were almost identical; therefore, of these, only cohort 1 is shown in Table 1. Cohort 3 differed from the other two across multiple categories, including performance status and interval between diagnosis and auto-HSCT. In all cohorts, 11.7% of patients presented with high-risk cytogenetics, and the majority of patients had at least a partial response or better at time of transplantation.
Table 1. Comparison of cohorts*
|
auto-HSCT, autologous hematopoietic stem cell transplant; CR, complete response; ISS, International Staging System; Mel140, 140 mg/m2 melphalan; Mel200, 200 mg/m2 melphalan; MR, minimal response; PR, partial response; prim refrac, primary refractory; prog, progression; rel, relapse; SD, stable disease; VGPR, very good partial response. |
|||
|
Characteristic, % |
Cohort 1: |
Cohort 3: |
p value |
|---|---|---|---|
|
Sex |
|
|
0.990 |
|
Male |
60.5 |
58.1 |
|
|
Female |
39.5 |
41.9 |
|
|
Age, years |
|
|
0.958 |
|
40−50 |
13.0 |
5.7 |
|
|
50−60 |
39.5 |
18.2 |
|
|
60−70 |
47.5 |
76.1 |
|
|
Time from diagnosis to auto-HSCT |
|
|
0.046 |
|
<6 months |
42.1 |
36.8 |
|
|
6−12 months |
57.9 |
63.2 |
|
|
Disease status at auto-HSCT |
|
|
<0.001 |
|
CR |
20.3 |
19.0 |
|
|
VGPR |
43.1 |
42.9 |
|
|
PR |
32.5 |
33.5 |
|
|
SD/MR |
2.5 |
2.6 |
|
|
Rel/prog/prim refrac |
1.6 |
1.9 |
|
|
ISS |
|
|
0.178 |
|
I |
40.1 |
24.0 |
|
|
II |
34.4 |
30.5 |
|
|
III |
25.5 |
45.4 |
|
|
Karnofsky score at auto-HSCT |
|
|
<0.001 |
|
≤70 |
5.5 |
8.1 |
|
|
80 |
19.8 |
27.3 |
|
|
90 |
40.9 |
40.7 |
|
|
100 |
33.8 |
24.0 |
|
|
High-risk cytogenetics |
|
|
<0.001 |
|
No/unknown |
88.3 |
88.3 |
|
|
Yes |
11.7 |
11.7 |
|
|
Tandem auto |
|
|
<0.001 |
|
No |
88.2 |
83.9 |
|
|
Yes |
1.8 |
16.1 |
|
Early relapse and PFS at 12 months are shown in Table 2 and are similar between groups.
Table 2. Cumulative incidence of early relapse and 12-month PFS*
|
PFS, progression free survival. |
||
|
Cohort |
Early relapse, % |
PFS, % |
|---|---|---|
|
1: Training |
14.7 |
84.1 |
|
2: Validation |
11.6 |
88.2 |
|
3: Validation |
16.9 |
80.3 |
Using Cox proportional hazard analysis, a scoring system was created with a score of 0−4. This score was created by assigning points according to each factors’ hazard ratio (HR), with higher points in factors associated with a higher risk of progression, i.e., higher HR. As shown in Figure 1, the sum of the score points is equal to the risk score, with the exception of scores ≥4, which give a risk score of 4.
Figure 1. Score calculation*
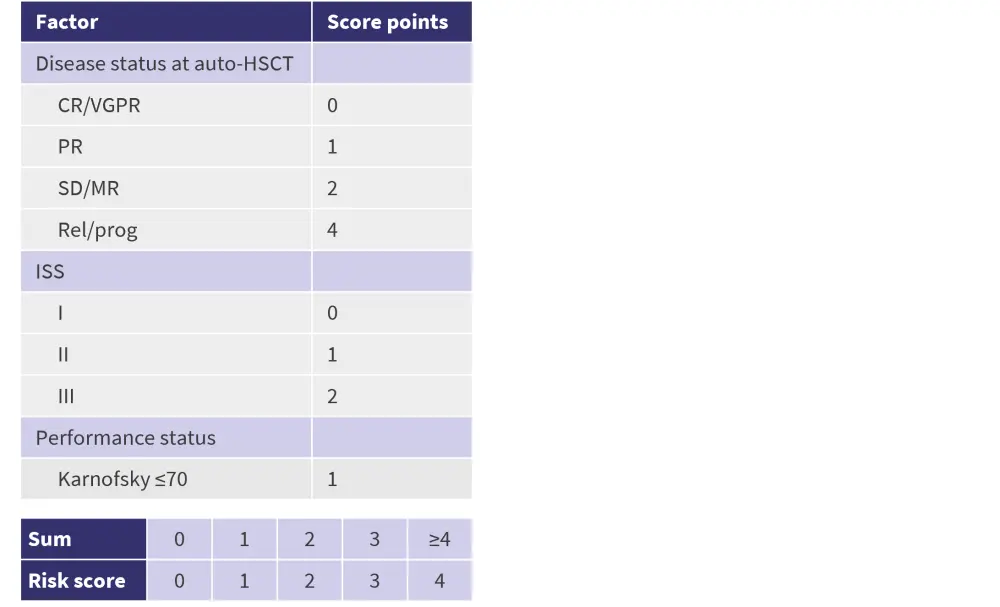
auto-HSCT, autologous hematopoietic stem cell transplantation; CR, complete response; HR, hazard ratio; ISS, International Staging System; MR, minimal response; PR, partial response; prog, progression; rel, relapse; SD, stable disease; VGPR, very good partial response.
*Adapted from Beksac.1
PFS was measured for each risk score within the three cohorts and was found to be significantly associated. The risk of relapse increased by 56% for every additional point in the score. In Table 3, the association between the score and the percentage of patients with early failure is shown across the three cohorts. The number of patients who experienced early failure increased in the subgroups with higher scores in all cohorts, showing the potential of this new scoring system as a prognostic factor.
Table 3. Score and early failure distribution across EBMT cohorts*
|
EBMT, European Society for Blood and Marrow Transplantation; Mel140, 140 mg/m2 melphalan; Mel200, 200 mg/m2 melphalan. |
|||||
|
Patients, % |
Score 0 |
Score 1 |
Score 2 |
Score 3 |
Score 4 |
|---|---|---|---|---|---|
|
Cohort 1 (Mel200 Training) |
24 |
34 |
30 |
10 |
3 |
|
Early failure† |
8.3 |
12.8 |
21.1 |
25.1 |
42.9 |
|
Cohort 2 (Mel200 Validation) |
25 |
36 |
29 |
8 |
2 |
|
Early failure† |
6.4 |
11.1 |
16.2 |
21.6 |
35.1 |
|
Cohort 3 (Mel140 Validation) |
15 |
25 |
38 |
17 |
5 |
|
Early failure† |
11 |
18.7 |
17.2 |
27.4 |
43.8 |
High-risk patients were evaluated separately, but the same trend was seen in this subgroup as before, with higher scores of the model being associated with a decreased 12-month PFS. The score was found to be predictive of early- and long-term survival (PFS and overall survival probability at 0–5 years).
To evaluate the sensitivity and specificity of this scoring system to predict early relapse, a dichotomized score was used.
- For patients with scores >1, this system has a specificity of 62% and a sensitivity of 60%.
- For patients with scores >3, the specificity improved to 98%, and the sensitivity was 7%.
Conclusion
This novel scoring system was developed using the EBMT database of >14,000 patients and uses readily accessible information, such as the disease status or the ISS stage, to calculate the final score, which facilitates its application in the clinic. Patients are split into five categories according to their risk of early relapse after HSCT, and a significant association was seen between the score value and survival outcomes. This score can be widely implemented since it was calculated using data from patients who received different induction and conditioning regimens and included patients undergoing tandem transplantation.
Expert Opinion
Using the EBMT score model, <5% of patients experienced a relapse and allowed for the prediction of not just early relapse but also 3-year overall survival. Currently, the EBMT model is based on ISS performance due to its high predictive ability; however, the hope is to replace this with the revised ISS or even MRD assessment and guidance, which would provide greater value in larger patient cohorts.
 Meral Beksaç
Meral BeksaçReferences
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?



