All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Mezigdomide + dexamethasone for the treatment of RRMM
Mezigdomide is an oral cereblon E3 ligase modulator which acts to degrade transcription factors Ikaros and Aiolos, ultimately resulting in multiple myeloma (MM) cell death. Mezigdomide is currently being investigated in combination with dexamethasone for the treatment of heavily pre-treated patients with MM.1
Here, we summarize key efficacy and safety data from the phase I and subsequent phase II trials (NCT03374085) of mezigdomide + dexamethasone combination therapy in patients with relapsed/refractory MM.
Phase I (Dose-escalation)1
The phase I dose-escalation study included 77 patients who had been treated with ≥3 prior lines of therapy. Four dosing schedules in 28-day cycles were assessed with the optimal dose brought forward to treat all patients in phase II.
Phase II (Dose-expansion)1
The phase II dose-expansion study included 101 patients with triple-class refractory MM. These patients were treated within 28-day cycles of mezigdomide/dexamethasone combination therapy following the recommended dosing schedule determined in phase I.
Patient characteristics1
A summary of the key baseline patient characteristics of the dose-escalation and dose-expansion cohorts are outlined in Table 1.
Table 1. Baseline patient characteristics*
|
ADC, antibody drug conjugate; BCMA, B-cell maturation antigen; CAR, chimeric antigen receptor; ECOG, Eastern Cooperative Oncology Group; IMiD, immunomodulatory agent; ISS, International Staging System; PI, proteasome inhibitor. |
||
|
Characteristic (%, unless otherwise specified) |
Dose-escalation cohort |
Dose-expansion cohort |
|---|---|---|
|
Median age (range), years |
65 (40–78) |
67 (42–85) |
|
Sex |
||
|
Male |
58 |
54 |
|
Female |
42 |
46 |
|
Race |
||
|
White |
90 |
76 |
|
Black |
4 |
4 |
|
Asian |
1 |
7 |
|
Other |
1 |
4 |
|
ISS stage |
||
|
I |
32 |
39 |
|
II |
44 |
41 |
|
III |
22 |
21 |
|
ECOG status score |
||
|
0 |
27 |
35 |
|
1 |
64 |
56 |
|
2 |
9 |
9 |
|
Cytogenetic high-risk |
30 |
37 |
|
Previous therapy |
||
|
Stem-cell transplant |
78 |
77 |
|
PI |
100 |
100 |
|
Lenalidomide |
99 |
100 |
|
Pomalidomide |
92 |
100 |
|
Anti-CD38 antibody |
78 |
100 |
|
Anti-BCMA therapy |
12 |
30 |
|
ADC |
9 |
22 |
|
T-cell engager |
1 |
8 |
|
CAR T-cell |
1 |
3 |
|
Refractory status |
||
|
IMiD |
95 |
100 |
|
Lenalidomide |
81 |
88 |
|
Pomalidomide |
84 |
96 |
|
PI |
75 |
100 |
|
Anti-CD38 antibody |
70 |
100 |
|
Triple-class |
56 |
100 |
Efficacy1
Dose-escalation cohort
In the dose-escalation cohort, two of the four regimens with highest overall response rates included:
- 1.0 mg mezigdomide in combination with dexamethasone administered once daily in 28-day cycles consisting of either:
- 21 days treatment, followed by a break of 7 days, or
- 10 days of treatment, followed by a break of 4 days
The final response data for all patients included in phase I, as well as data for each of the above regimens are outlined in Figure 1. Ultimately, the 21-day cycle dosing regimen was elected as optimal and carried forward to all patients in the subsequent dose-expansion trial.
Figure 1. Response rates in the dose-escalation cohort*
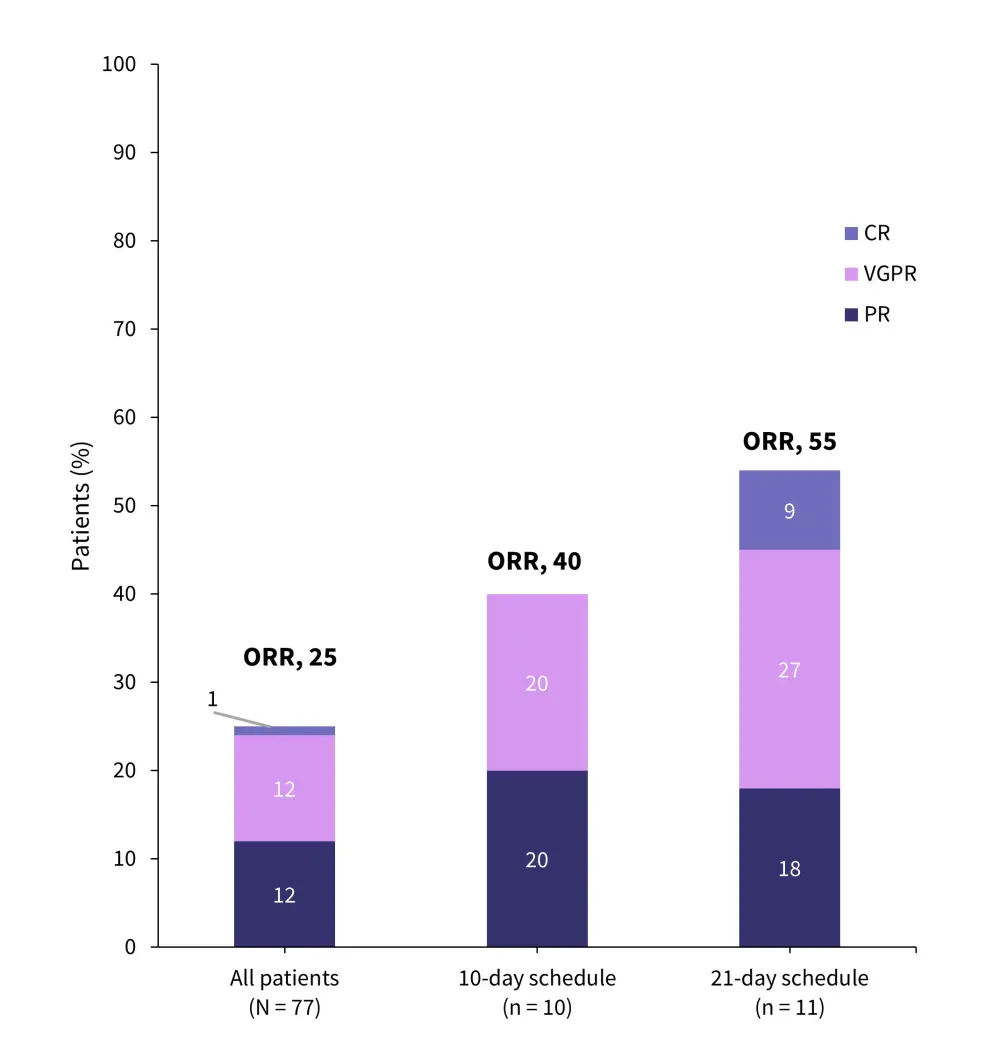
CR, complete response; ORR, overall response rate; PR, partial response; VGPR, very good partial response.
*Data from Richardson, et al.1
Dose-expansion cohort
At a median follow up of 7.5 months, an overall response rate of 41% was observed across the whole cohort. A subset of patients treated with a previous BCMA-targeted therapy presented with an overall higher response rate of 50% (Figure 2.). However, stringent complete response was not reached by any of these patients versus 2% of patients with no prior anti-BCMA therapy.
Figure 2. Response rates in the dose-expansion cohort*
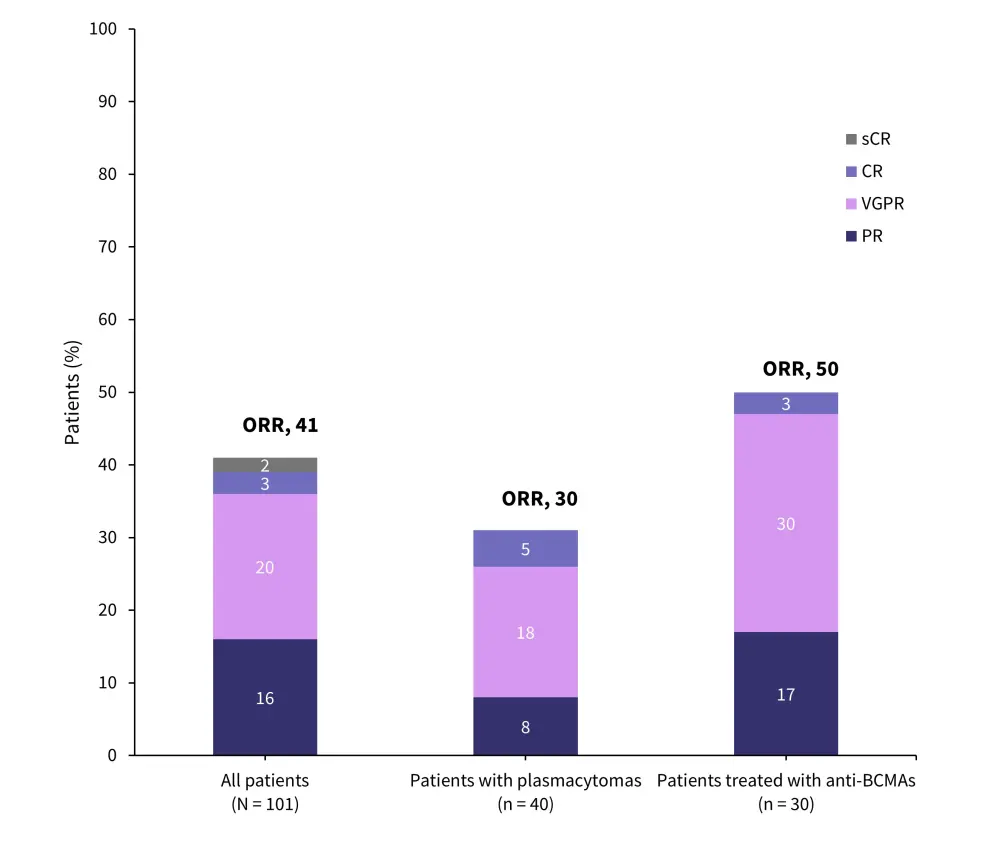
CR, complete response; ORR, overall response rate; PR, partial response; sCR, stringent complete response; VGPR, very good partial response.
*Data from Richardson, et al.1
Additional data on responses in the total dose-expansion cohort includes:
- Median duration of response, 7.6 months
- Median progression-free survival, 4.4 months
- Stable disease, 39%
- Progressive disease, 10%
Safety1
The most common adverse events in both the dose-escalation and dose-expansion cohorts were hematologic. Neutropenia was the most common, occurring in 81% and 77% of patients in dose-escalation and dose-expansion cohorts, respectively. All Grade ≥3 adverse events in both cohorts are shown in Figure 3.
Figure 3. Grade ≥3 adverse events in the dose-escalation and dose-expansion cohorts*
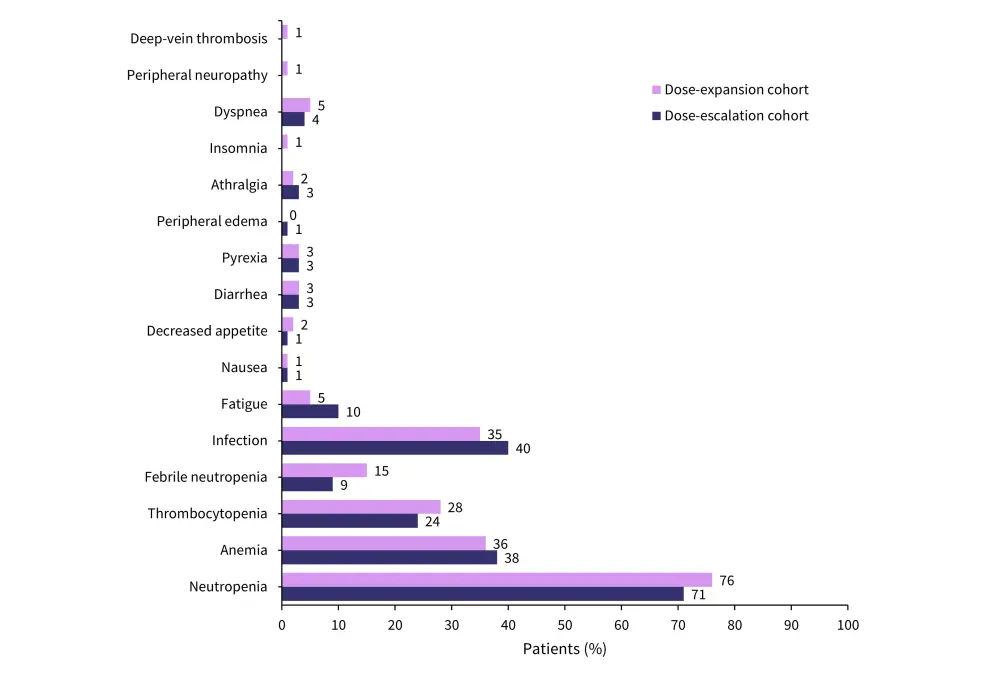
*Data from Richardson, et al.1
Conclusion
Mezigdomide combined with dexamethasone in patients with triple-class refractory MM resulted in safety and efficacy data deemed favorable by researchers. However, it is important to note that the phase II part of this trial was single-armed; therefore, comparisons between the intervention versus no therapy or standard-of-care therapies was not established. Nonetheless, the data from the trial does present a feasible dosing regimen and the basis for further research.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?

