All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Managing thrombosis in multiple myeloma: Expert recommendations
The approval of novel therapeutic agents for multiple myeloma (MM), including proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies, has improved patient outcomes.1 However, the introduction of these agents has also altered the frequency and epidemiology of thrombotic events. Thrombosis currently represents a significant cause of morbidity and mortality in patients with MM, and thromboprophylaxis is suboptimal.1
The Multiple Myeloma Hub previously reviewed the risks of thrombosis and the recommended thromboprophylaxis in MM. Here, we summarize practical aspects of recommendations for thrombotic risk factors and risk stratification, primary thromboprophylaxis, management of acute thrombotic events, and secondary thromboprophylaxis, as published by an expert panel in Haematologica.1
Thrombohemorrhagic risk factors and risk stratification
All patients with MM who are candidates for treatment require a thrombosis risk evaluation to prevent thromboembolic complications. Evaluations should include patient, disease, and treatment-related risk factors (Figure 1).
Figure 1. Key thrombosis risk factors in MM*
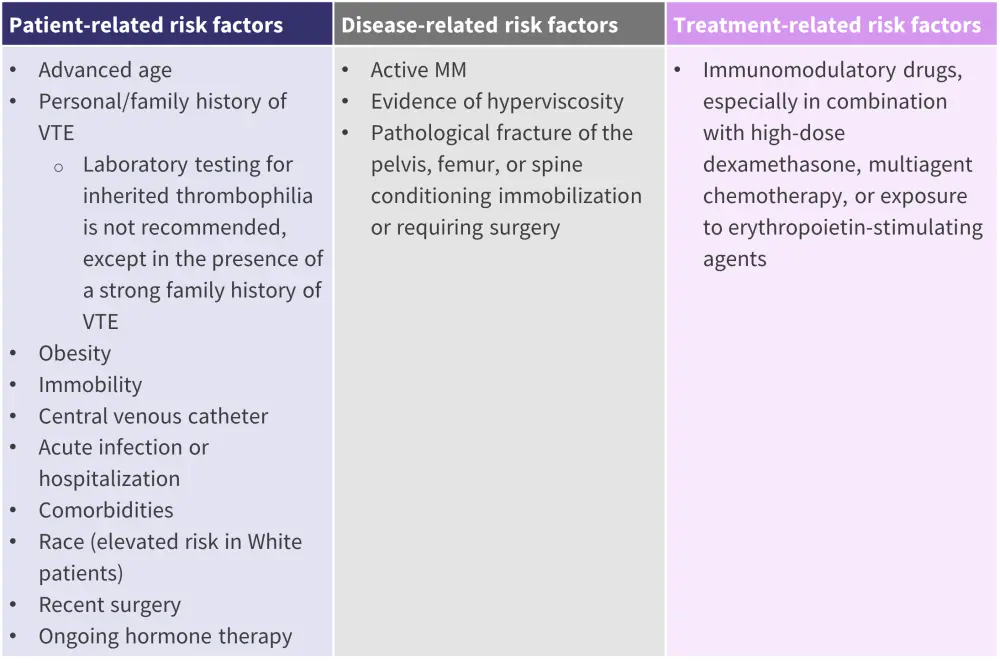
MM, multiple myeloma; VTE, venous thromboembolism.
*Adapted from De Stefano, et al.1
There are insufficient data to recommend one specific risk assessment model in clinical practice. Application of a risk assessment model should be consistent for all patients in a single center.
In addition to thrombotic risk assessment, bleeding risk should be assessed before initiation of anti-myeloma therapy.
- An accurate patient history should be obtained, and bleeding history investigated.
- Prothrombin time, partial thromboplastin time, platelet count, and fibrinogen level should be evaluated.
- Patients with primary diagnostic test results indicative of a bleeding predisposition, or with a history of bleeding, should be evaluated by secondary diagnostic tests in cooperation with a coagulation expert.
Primary antithrombotic prophylaxis in patients with MM
All patients with MM eligible for anti-myeloma treatment should be considered for thromboprophylaxis. Thromboprophylaxis type, intensity, and duration should be tailored according to individual baseline thrombotic and hemorrhagic risk profiles. Contraindications for thromboprophylaxis are shown in Figure 2.
Figure 2. Contraindications for thromboprophylaxis*
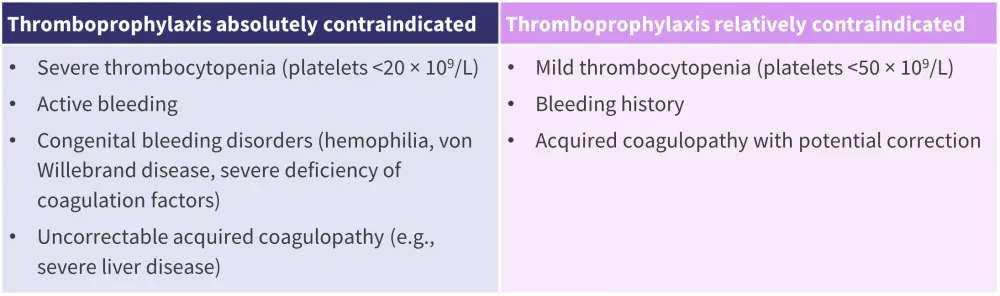
*Adapted from De Stefano, et al.1
Considerations for determining appropriate primary antithrombotic prophylaxis in selected patient subpopulations are outlined in Figure 3.
Figure 3. Considerations for primary antithrombotic prophylaxis in selected patient subpopulations with MM*
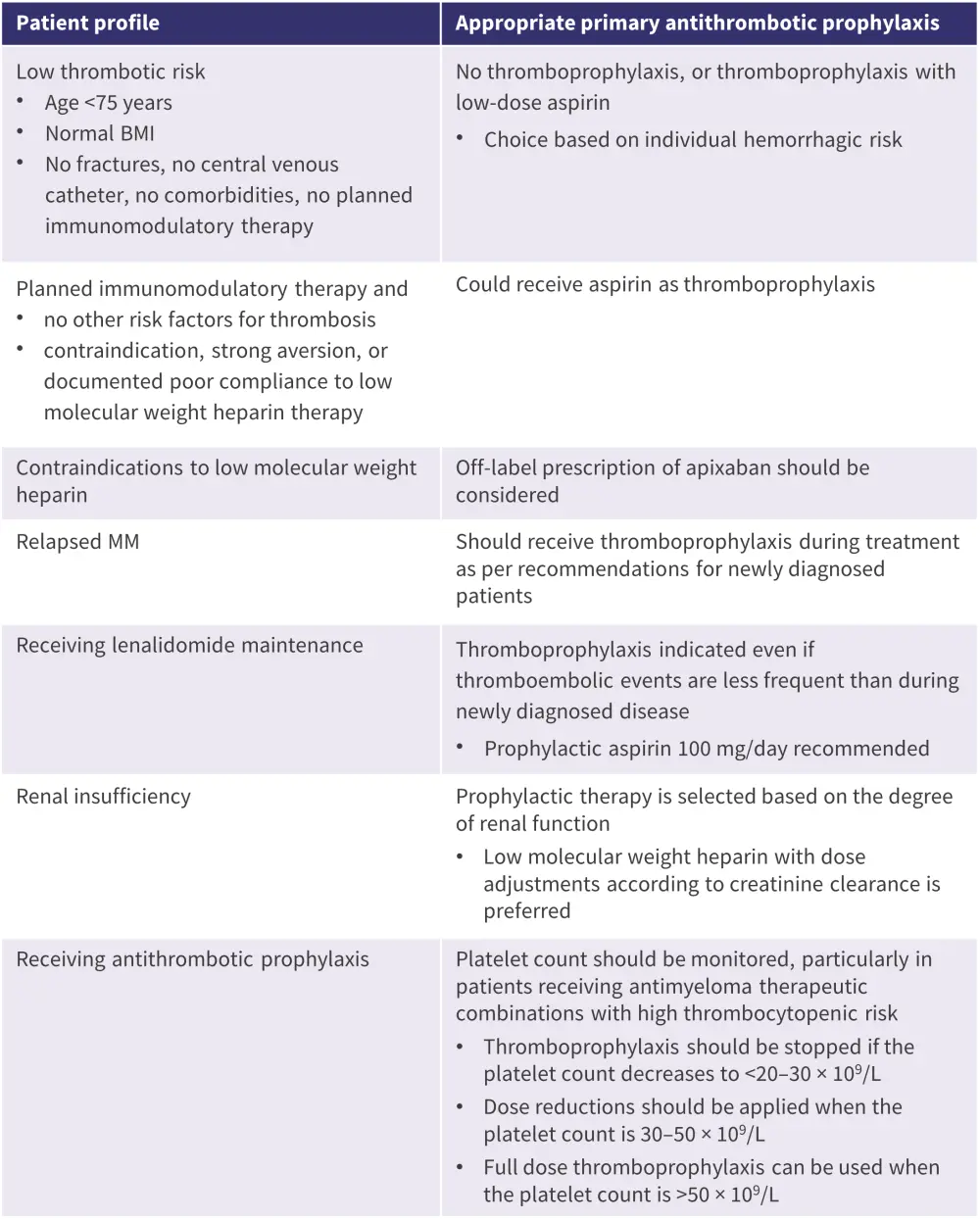
BMI, basal metabolic index; MM, multiple myeloma.
*Adapted from De Stefano, et al.1
- Thromboprophylaxis should be prescribed to all other patients, with low molecular weight heparin as the preferred initial option.
- Thromboprophylaxis duration should be modulated according to anti-myeloma treatment duration and evolving risk factors.
- Prophylaxis should continue whilst thrombosis presents a risk (e.g., active disease or assumption of drugs with a thrombotic risk).
- Primary thromboprophylaxis should be stopped in case of major or clinically relevant bleeding.
- In this circumstance, the cause of bleeding should be evaluated and corrected before reinitiating thromboprophylaxis.
- Other considerations include drug–drug interactions and patient preference and compliance.
Early treatment of acute thrombotic events, secondary antithrombotic prophylaxis, and re-exposure to anti-myeloma drug in patients with MM
In general, acute thrombosis treatment during active MM treatment should not differ from standard recommendations. Considerations for determining appropriate secondary antithrombotic prophylaxis in selected patient subpopulations are outlined in Figure 4.
Figure 4. Considerations for secondary antithrombotic prophylaxis in selected patient subpopulations*
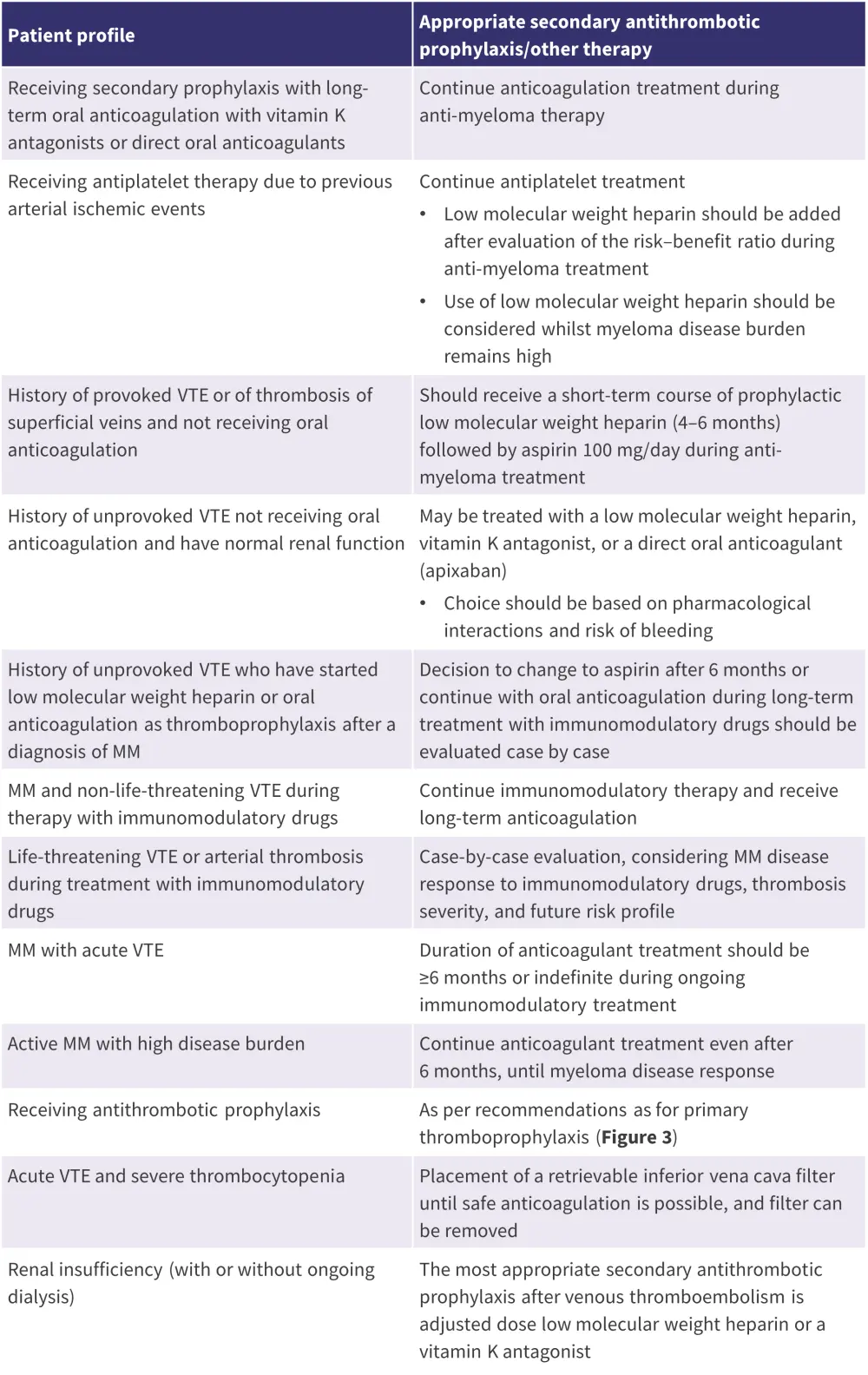
MM, multiple myeloma; VTE, venous thromboembolism.
*Adapted from De Stefano, et al.1
Conclusion
De Stefano et al. provide general recommendations for thrombosis management in MM, as well as recommendations for key patient subpopulations. The expert panel advise that all patients with MM requiring treatment should receive a thrombosis risk evaluation to prevent thromboembolic complications. The evaluation should include patient, disease, and treatment-related risk factors, and concomitant bleeding risk assessment. Recommendations for primary antithrombotic prophylaxis, early treatment of acute thrombotic events, secondary antithrombotic prophylaxis, and re-exposure to anti-myeloma drugs are based on patient profile. These recommendations aim to minimize the risk of thrombosis and maximize treatment adherence in patients with MM who require active treatment.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?



