All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Final results from the PLEIADES and EQUULEUS trials: Daratumumab, carfilzomib, and dexamethasone in RRMM
Daratumumab, carfilzomib, and dexamethasone (D-Kd) is an approved standard combination regimen for the treatment of adult patients with relapsed/refractory multiple myeloma (RRMM).1 Positive results from the phase III CANDOR trial (NCT03158688) led to the U.S. Food and Drug Administration (FDA) approval of D-Kd with intravenous (IV) daratumumab plus twice weekly carfilzomib (56 mg/m2) following one to three prior lines of therapies.1,2 The updated efficacy and safety data were reported on the Multiple Myeloma Hub here.
When carfilzomib (70 mg/m2) is administered once weekly, it offers a more convenient regimen for patients with RRMM, exhibiting promising responses with both subcutaneous (SC) and IV daratumumab in the initial analyses of the phase II PLEIADES (NCT03412565) and phase Ib EQUULEUS (NCT01998971) trials, respectively. These preliminary data resulted in the U.S. FDA approval of once weekly carfilzomib with both SC and IV daratumumab. Herein, we report the final analysis of both trials published by Moreau et al.1 in the Blood Cancer Journal.
Results from the PLEIADES and EQUULEUS trials1
Overall, D-Kd was administered to 66 patients in the PLEIADES trial following one prior line of lenalidomide-based therapy and to 85 patients in EQUULEUS after one to three previous lines of therapy. The median prior lines of therapy were one and two for PLEIADES and EQUULEUS, respectively; baseline characteristics for the two studies are summarized in Table 1.
Table 1. Selected baseline characteristics for the PLEIADES and EQUULEUS trials*
|
ECOG, Eastern Cooperative Oncology Group; IMiD, immune-mediated inflammatory disease; PI, proteasome inhibitor. |
||
|
Characteristic, % (unless otherwise stated) |
PLEIADES |
EQUULEUS |
|---|---|---|
|
Median age (range), years |
61 (42–84) |
66 (38–85) |
|
ECOG performance status |
|
|
|
0 |
60.6 |
37.6 |
|
1 |
34.8 |
54.1 |
|
2 |
4.5 |
8.2 |
|
Refractory to† |
|
|
|
Lenalidomide |
62.1 |
60.0 |
|
Pomalidomide |
0.0 |
12.9 |
|
Bortezomib |
7.6 |
30.6 |
|
PI + IMiD |
13.6 |
29.4 |
|
Last prior line of therapy |
62.1 |
63.5 |
|
Cytogenetics‡ |
|
|
|
High risk |
36.4 |
19.4 |
|
Standard risk |
63.6 |
80.6 |
Updated efficacy
PLEIADES
The following results were observed at the median follow-up of 12.4 months in the PLEIADES trial:
- The overall response rate (ORR) was 84.8% in the total cohort and 84.1% in the lenalidomide-refractory cohort.
- The ORR was 75% and 82.1% in the high-risk versus standard-risk cytogenetic cohorts, respectively.
- Median duration of response (DoR) was not reached; the 9-month DoR was 85.4%
- Progression-free survival (PFS) and overall survival (OS) were not assessed.
EQUULEUS
In the EQUULEUS trial, at the median follow-up of 23.7 months, the median DoR was 27.5 months, with a 9-month DoR of 88.3%, and median OS was not reached, with a 24-month OS of 71.2%. The following was observed for the overall population versus lenalidomide-refractory cohorts:
- The ORR was 81.2% vs 74.5%, respectively.
- The median PFS was 25.7 months vs 22.3 months, respectively.
- The 24-month PFS was 52.7% vs 46.9%, respectively.
Updated safety results in PLEIADES and EQUULEUS
Any grade treatment-emergent adverse events (TEAEs) occurred in all patients within the PLEIADES and EQUULEUS trials, with Grade 3–4 TEAEs reported in 74.2% and 78.8% of patients in PLEIADES and EQUULEUS, respectively. The most common any grade and Grade 3–4 hematologic and nonhematologic TEAEs in both trials are reported in Table 2.
Table 2. Any grade (≥25%) and Grade 3–4 (≥5%) TEAEs in the PLEIADES and EQUULEUS trials*
|
TEAE, treatment-emergent adverse event. |
||||
|
TEAE, % |
PLEIADES |
EQUULEUS |
||
|---|---|---|---|---|
|
Any grade |
Grade 3–4 |
Any grade |
Grade 3–4 |
|
|
Hematologic |
|
|
|
|
|
Thrombocytopenia |
51.5 |
19.7 |
68.2 |
31.8 |
|
Anemia |
37.9 |
12.1 |
51.8 |
21.2 |
|
Neutropenia |
22.7 |
10.6 |
30.6 |
21.2 |
|
Lymphopenia |
18.2 |
12.1 |
29.4 |
24.7 |
|
Nonhematologic |
|
|
|
|
|
Hypertension |
34.8 |
21.2 |
32.9 |
20.0 |
|
Insomnia |
34.8 |
6.1 |
32.9 |
4.7 |
|
Diarrhea |
30.3 |
0.0 |
37.6 |
2.4 |
|
Nausea |
25.8 |
0.0 |
42.4 |
1.2 |
|
Nasopharyngitis |
25.8 |
0.0 |
17.6 |
0.0 |
|
Headache |
22.7 |
0.0 |
27.1 |
1.2 |
|
Pyrexia |
21.2 |
1.5 |
36.5 |
1.2 |
|
Asthenia |
21.2 |
0.0 |
42.4 |
15.3 |
|
Cough |
19.7 |
0.0 |
28.2 |
0.0 |
|
Dyspnea |
18.2 |
1.5 |
35.3 |
3.5 |
|
Upper respiratory tract infection |
18.2 |
0.0 |
44.7 |
3.5 |
|
Vomiting |
16.7 |
0.0 |
40.0 |
1.2 |
Additional adverse events reported in the PLEIADES and EQUULEUS trials are shown in Table 3.
Table 3. Specific TEAEs in the PLEIADES and EQUULEUS trials*
|
IRR, infusion-related reactions; IV, intravenous; NR, not reported; SC, subcutaneous; TEAE, treatment-emergent adverse event. †Most commonly pneumonia in both trials and basal cell carcinoma and upper respiratory tract infection in EQUULEUS. |
||
|
TEAE, n (unless otherwise stated) |
PLEIADES |
EQUULEUS |
|---|---|---|
|
Grade 3–4 infections, % |
13.6 |
21.2 |
|
Serious TEAE, %† |
33.3 |
48.2 |
|
Grade 5 TEAE‡ |
3 |
3 |
|
Treatment discontinuation due to a TEAE |
1 |
5 |
|
Grade 3–4 cardiac TEAEs§ |
2 |
9 |
|
IRR‖ |
|
|
|
After first SC or IV |
3 |
6 |
|
After split first dose |
NR |
31 |
Recommended dosing regimens of D-Kd in adult patients with RRMM1,3,4
The recommended dosage regimens for IV or SC daratumumab, the two-dosing (50 mg/m2 twice weekly or 70 mg/m2 once weekly) carfilzomib schema, and dexamethasone when administered in combination are presented in Figure 1.
Figure 1. Dosing schedule for the D-Kd regimen in RRMM*
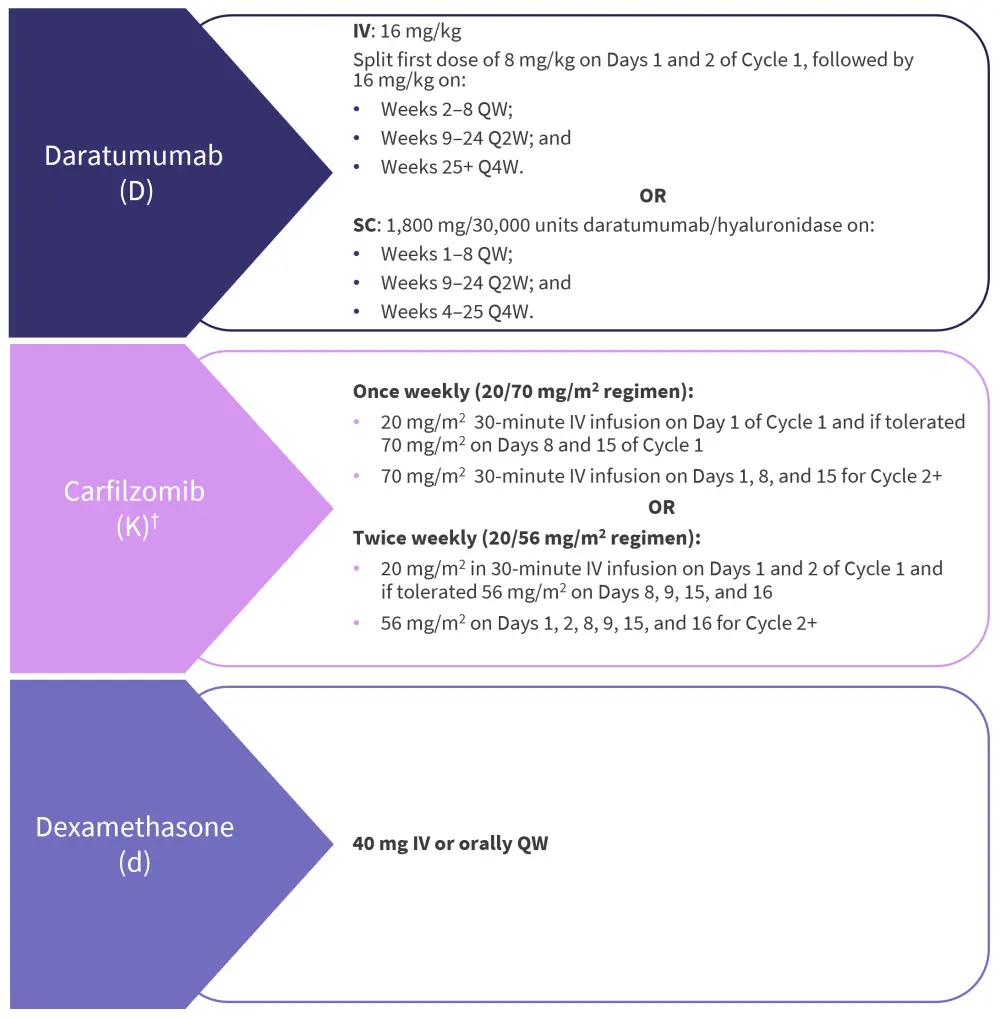
IV, intravenous; Q2W, every two weeks; Q4W, every four weeks; QW, weekly; SC, subcutaneous.
*Data from Moreau, et al.1 and U.S. Food and Drug Administration.3,4
†Based on 28-day cycles.
Conclusion
In the longer follow-up analyses of PLEIADES and EQUULEUS, D-Kd regimens were efficacious and well-tolerated in patients with RRMM both in the all-treated and lenalidomide-refractory cohorts. Despite the small sample sizes, these final data further support the use of D-Kd as a standard treatment regimen in RRMM.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?




