All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Final analysis from phase III CANDOR trial in adult patients with RRMM
Do you know... The primary endpoint of the phase III CANDOR trial was progression-free survival (PFS), which was met in the primary analysis. What was the median PFS in patients with relapsed/refractory MM treated with carfilzomib + daratumumab + dexamethasone in the final analysis?
Survival outcomes in patients with multiple myeloma (MM) have improved significantly due to novel agents such as monoclonal antibodies and immunomodulatory drugs. Despite these improvements, MM remains generally incurable.1 Currently, lenalidomide is one of the most common front-line therapies administered to patients. However, lenalidomide is often administered until disease progression, resulting in patients becoming refractory to the therapy.1 The need for alternative treatment strategies is important in ensuring optimal clinical outcomes for these patients.
The phase III CANDOR trial (NCT03158688) investigated the efficacy of carfilzomib + daratumumab + dexamethasone (KdD) versus carfilzomib + dexamethasone (Kd) in adult patients with relapsed or refractory (R/R) MM. The primary analysis reported that the trial met its primary endpoint of progression-free survival (PFS). The interim analysis demonstrated that the KdD regime continued to show higher median PFS. Recently, Usmani et al. published the final analysis of the CANDOR trial in Blood Advances with updated safety and efficacy data.1 We summarize the key findings here.
Study design
This was a randomized, multicenter, open-label, phase III trial in patients aged ≥18 years with RRMM, who had an Eastern Cooperative Oncology Group performance status of 0–2 and had received 1–3 prior lines of therapy. Baseline patient characteristics have previously been reported by the MM Hub. The dosing schedule is highlighted in Figure 1.
Pre-defined patient subgroups included in the analysis were based on the number of prior therapies, as well as exposure and/or refractory to protease inhibitors or immunomodulatory drugs including lenalidomide.
Figure 1. Dosing schedule*
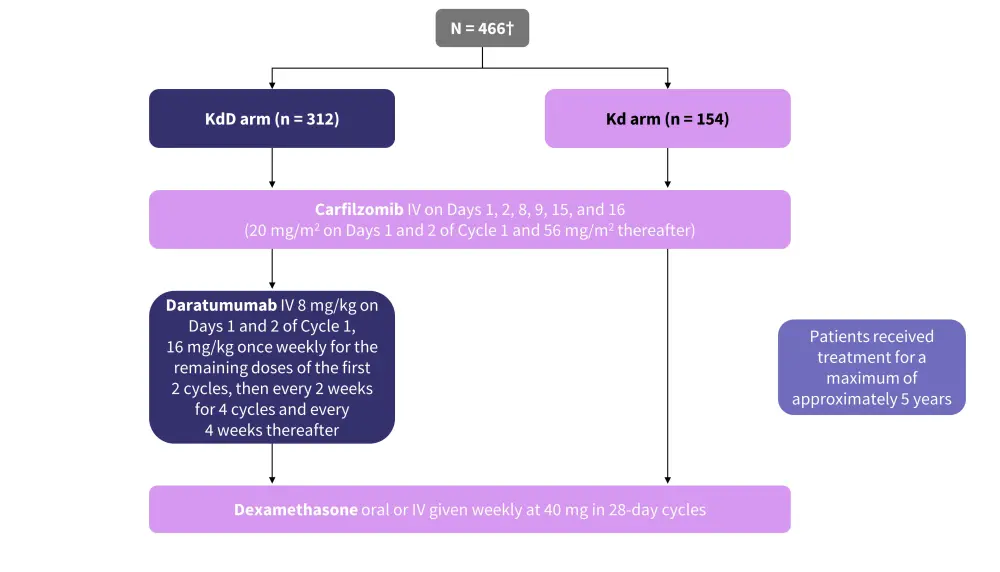
IV, intravenous; Kd, carfilzomib + dexamethasone; KdD, carfilzomib + daratumumab + dexamethasone.
*Adapted from Usmani, et al.1
†Randomization was stratified based on the international staging system at screening, previous protease inhibitor exposure, number of previous lines of therapy, and previous anti-CD38 monoclonal antibody therapy.
The primary endpoint was PFS, defined as the time from randomization until disease progression or death from any cause. Disease progression was assessed every 28 ± 7 days based on the International Myeloma Working Group criteria. The key secondary endpoints included overall response rate and minimal residual disease (MRD) negativity.
Results
Efficacy
A total of 466 patients were included: 312 in the KdD and 154 in the Kd arm. The median follow-up times were 50.6 and 50.1 months in the KdD and Kd arms, respectively.
- The rates of MRD negativity at 12 months was three-fold higher in patients in the KdD versus the Kd arm (Figure 2).
- Median PFS was higher in the KdD arm compared with the Kd arm (28.4 vs 15.2 months; hazard ratio [HR], 0.64).
- Median overall survival was 50.8 versus 43.6 months in the KdD and Kd arms, respectively (HR, 0.78; p = 0.042).
- There was a trend towards improved overall survival in the KdD versus the Kd arm in several patient subgroups, including:
- Patients refractory to lenalidomide (not reached vs 38.2 months; HR, 0.69)
- Patients refractory to proteasome inhibitor (43.2 vs 30 months; HR, 0.70)
- Patients in KdD arm with high-risk cytogenetics (HR, 0.52) and International Staging System III at screening (HR, 0.58) showed a significant improvement in overall survival.
- The median time to next treatment was higher in the KdD arm compared with the Kd arm (37.4 vs 17.8 months).
Figure 2. Rates of MRD negativity with KdD*
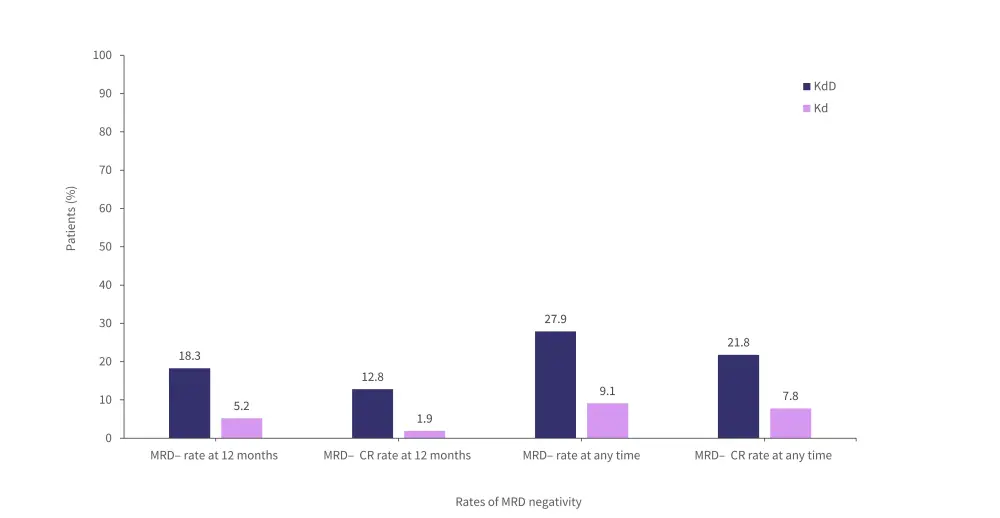
CR, complete response; Kd, carfilzomib + dexamethasone; kdD, carfilzomib + daratumumab + dexamethasone; MRD–, measurable residual disease negative.
*Adapted from Usmani, et al.1
Safety
- Safety outcomes were comparable across treatment arms (Table 1) and were consistent with the outcomes of previous analyses.
Table 1. Treatment-emergent adverse events*
|
Kd, carfilzomib + dexamethasone; KdD, carfilzomib + daratumumab + dexamethasone; TEAE, treatment-emergent adverse event. *Adapted from Usmani, et al.1 |
||
|
TEAE, (% unless otherwise stated) |
KdD (n = 312) |
Kd (n = 154) |
|---|---|---|
|
Any-grade TEAE |
99 |
97 |
|
Grade ≥3 TEAE |
87 |
78 |
|
Serious TEAE |
68 |
52 |
|
Fatal TEAE |
11 |
6 |
|
Study discontinuations due to TEAE |
34 |
27 |
- The most frequently experienced hematologic and non-hematologic treatment-emergent adverse events of any grade are shown in Figure 3.
- Since the primary analysis, no new fatal treatment-related adverse events were reported.
Figure 3. Most frequently occurring TEAE of any grade experienced by ≥20% of patients*
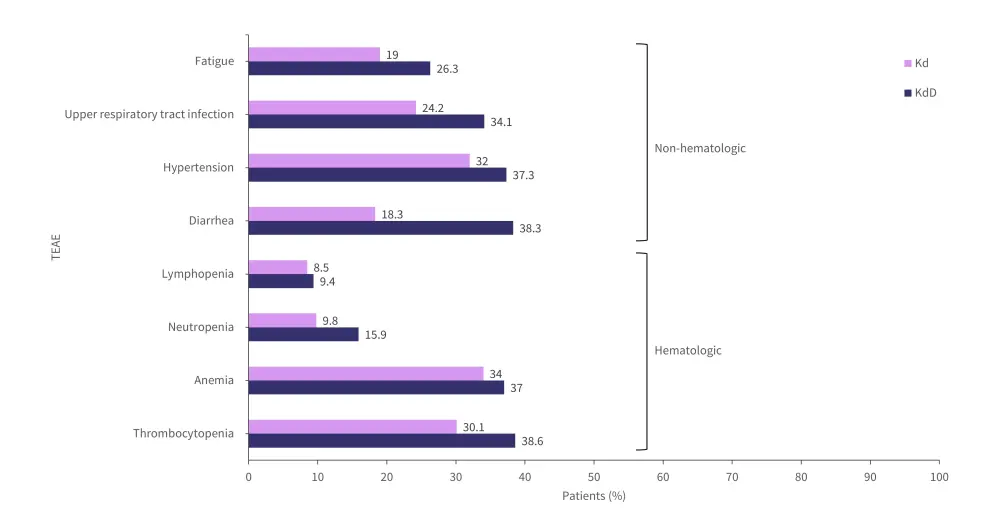
Kd, carfilzomib + dexamethasone; KdD, carfilzomib + daratumumab + dexamethasone; TEAE, treatment-emergent adverse event.
*Adapted from Usmani, et al.1
Conclusion
The final analysis of the CANDOR trial shows a significantly improved PFS as well as a trend towards improved overall survival in patients treated with KdD. Patients in the KdD arm also showed a consistently higher rate of MRD negativity compared with those in the Kd arm. Overall, the favorable risk-benefit profile of KdD regimen strengthens the rationale for its use as standard of care, particularly in patients who are refractory to lenalidomide or have high-risk cytogenetics.
However, the results of this trial should be interpreted in the context of certain limitations. Firstly, assessment of outcomes was challenging due to the small proportion of patients aged ≥75 years. Furthermore, there were many patients with unknown cytogenetics, which also made it difficult to assess clinical outcomes.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?




