All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
CAR T-cell therapy in older patients: Efficacy and rates of immune-mediated toxicity
Older patients (≥ 65 years) diagnosed with multiple myeloma (MM) are under-represented in clinical trials evaluating anti B-cell maturation antigen-directed chimeric antigen receptor (BCMA CAR) T-cell therapy, and are prone to inferior clinical outcomes due to associated comorbidities and reduced functional reserves.1
Akhtar et al.1 published a systematic review and meta-analysis investigating the efficacy of CAR T-cell therapies and rates of associated immune-mediated toxicity in older patients with MM. We summarize the key findings below.
Methods1
- The review encompassed phase I, II, and III clinical trials and prospective observational studies including patients ≥65 years old with MM or plasma cell leukemia and receiving anti-BCMA CAR T-cell therapy.
- PubMed, Scopus, Web of Science, Ovid, Embase, CENTRAL, and CINAHL databases were screened.
- Case reports, case series, and retrospective studies were excluded.
Key findings1
- A total of 14 studies were analyzed (N = 558):
- 3 studies were phase II (n = 287).
- 10 studies were phase I (n = 266).
- 1 study was a prospective, observational study (n = 5).
- Overall response rates (ORR) were high in the older patient population (Figure 1) and remained comparable to younger patients <60 years old (86%).
Figure 1. Pooled ORR in older patients treated with anti-BCMA CAR T-cell therapy*
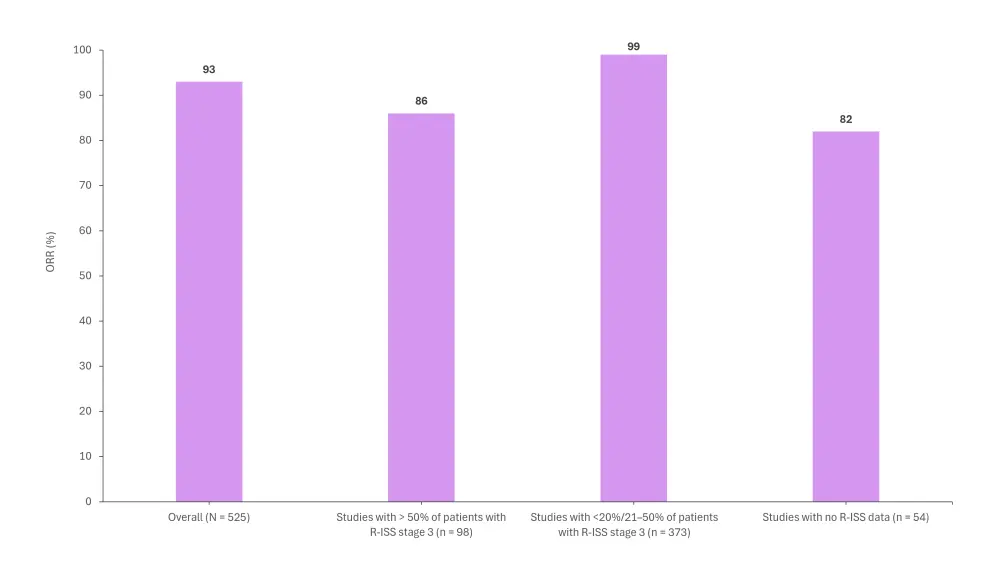
ORR, overall response rate; R-ISS, revised-international staging system.
*Adapted from Akhtar, et al.1
- Information on cytokine release syndrome (CRS) was available in 335 patients.
- The pooled CRS rate in older patients was 95%, compared with 91% in younger patients.
- Grade ≥3 CRS occurred in 21% of older patients vs 20% in younger patients.
- Information on immune cell-associated neurotoxicity syndrome (ICANS) was available in 316 patients.
- The pooled rate of ICANS in older patients was 15% compared with 6% in younger patients.
- Pooled rates of Grade ≥3 ICANS were comparable between older and younger patients, at 1% and 0%, respectively.
|
Key learnings |
|---|
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?




