All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Visual abstract | Key updates to the classification of plasma cell neoplasms and paraprotein disorders: The 5th WHO Classification
Do you know... Which of the following is a diagnostic feature of AESOP syndrome?
The Multiple Myeloma Hub is pleased to present a visual abstract highlighting key updates and changes in the 5th edition of the World Health Organization (WHO) Classification of Haematolymphoid Tumours,1 focussing on plasma cell neoplasms and paraprotein-producing disorders.
The latest update reflects changes in the reclassification of some conditions.2 Several new conditions have been added, including AESOP syndrome, TEMPI syndrome (which was a provisional entry in the 4th edition), cold agglutinin disease, and monoclonal gammopathy of renal significance (the subtypes of which are detailed in Table 1).
Furthermore, a number of sections have been reorganized, for example, IgM and non-IgM monoclonal gammopathy of unknown significance and monoclonal gammopathy of renal significance have been grouped as monoclonal gammopathies, diseases with abnormal monoclonal immunoglobulin deposits have been classified together, and heavy chain diseases are now included as plasma cell disorders.2
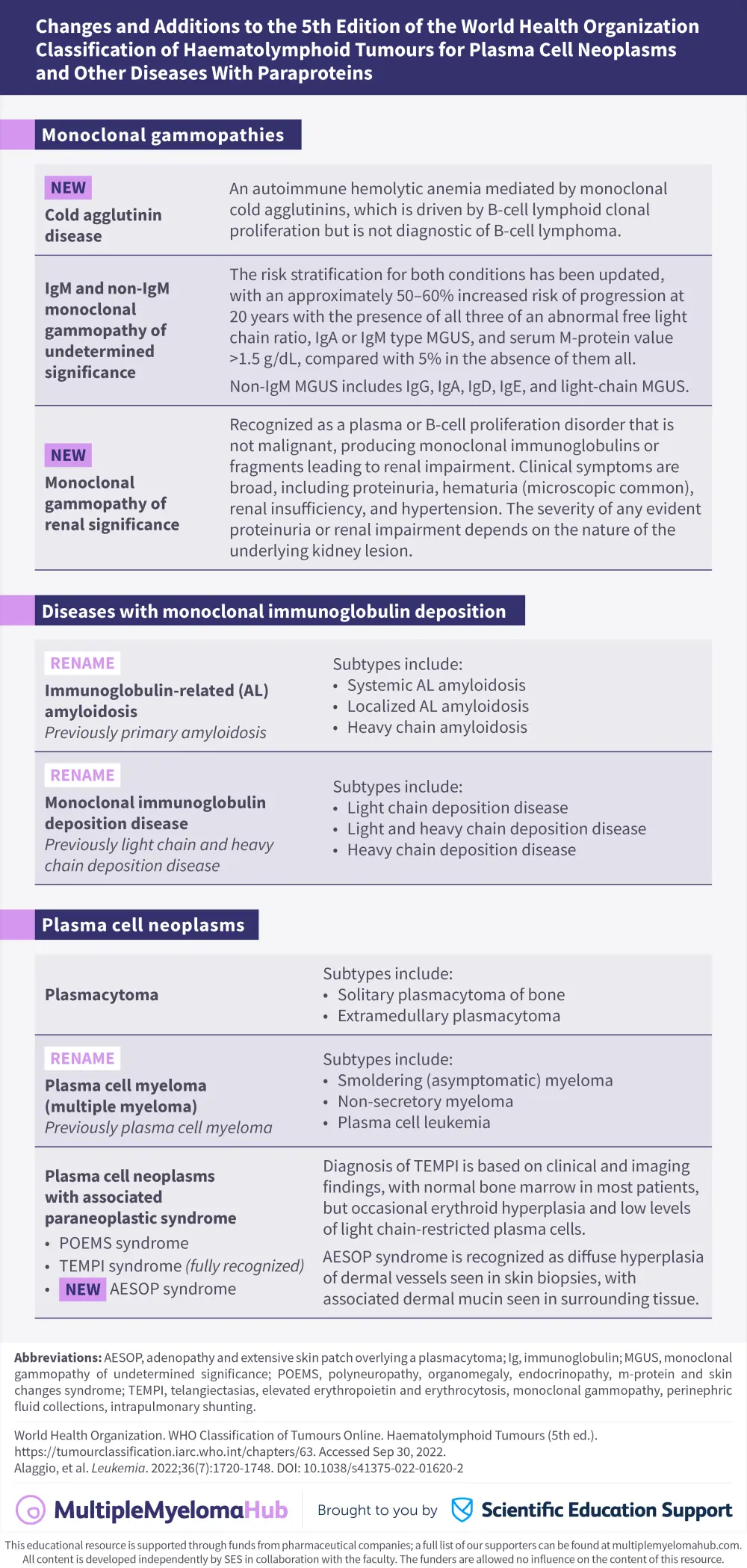
Table 1. MGRS subtypes according to the 5th edition of the World Health Organization Classification of Haematolymphoid Tumours*
|
GBM, glomerular basement membrane; HC, heavy chain; Ig, immunoglobulin; LC, light chain; MG, monoclonal gammopathy; MIg, monoclonal immunoglobulin; MRGS, monoclonal gammopathy of renal significance; TMA, thrombotic microangiopathy. |
|||
|
Subtype |
Ig deposits |
Immunological and ultrastructural characteristics |
Extrarenal manifestations |
|---|---|---|---|
|
Always associated with MGRS |
|||
|
Crystal storing histiocytosis |
LC |
Intracellular LC crystals in interstitial histiocytes (with or without crystals in tubular and glomerular cells |
Yes |
|
Crystalglobulin-induced nephropathy |
Ig |
Extracellular MIg crystals within glomerular and vessel lumina (with or without TMA) |
Yes |
|
Ig-related amyloidosis |
LC, Ig, HC |
Extracellular deposition of Congophilic randomly-oriented fibrils |
Yes |
|
Light chain proximal tubulopathy |
LC |
Crystalline or non-crystalline LC inclusions within proximal tubular cells |
Yes |
|
Monoclonal immunoglobulin deposition disease |
LC, Ig, HC |
Finely granular “punctate” MIg deposits in tubular and glomerular basement membranes and mesangium |
Yes |
|
Proliferative glomerulonephritis with monoclonal immunoglobulin deposits |
Ig, LC |
Amorphous MIg deposits in mesangium and subendothelial zone (and occasionally in subepithelial zone) |
No |
|
Frequently associated with MGRS |
|||
|
C3 glomerulopathy with MG |
Only C3 |
C3 deposits in mesangium, subendothelial and subepithelial zones (and the lamina densa of the glomerular basement membranes in dense deposit disease) |
No |
|
Cryoglobulinemic glomerulonephritis (Type I and most II) |
Ig |
Short microtubular and annular deposits composed of MIg only or MIg and polyclonal Igs |
Yes |
|
Monoclonal immunotactoid glomerulonephritis |
Ig |
Microtubular deposits composed of MIg |
No |
|
Thrombotic microangiopathy with MG |
None |
Chronic endothelial cell injury, no MIg or C3 deposits |
Yes |
|
Rarely associated with MGRS |
|||
|
Monotypic membranous nephropathy |
Ig |
Subepithelial deposits of MIg |
No |
|
Monotypic anti-GBM disease |
Ig |
Linear deposits of MIg along the glomerular basement membranes, no electron dense deposits ultrastructurally |
No |
|
Monotypic IgA nephropathy/ Henoch Schönlein purpura nephritis |
Ig |
Monoclonal IgA deposits in the mesangium ((and occasionally in subepithelial and/or subepithelial zones) |
No/yes |
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?

