All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
The impact of physical activity on functional performance in multiple myeloma
Do you know... What was the most common adverse event associated with physical activity in patients with multiple myeloma?
As treatments for multiple myeloma (MM) improve, patients are experiencing longer remissions. As a result, patients are expressing more interest in returning to activities of daily life, including physical activity (PA), sports, and hobbies. However, MM-associated bone disease has led to reluctance among physicians to recommend PA for MM patients due to the risk of new fractures that could impact frailty status.1
At the 20th International Myeloma Society (IMS) Annual Meeting, Hillengass presented findings on the impact of PA on functional performance and quality of life in patients with MM. The Multiple Myeloma Hub is pleased to summarize this presentation here.
Study design1
Over 6 months, 42 patients from a single center were given a choice of participating one of the following cohorts:
- Resistance (strength) training cohort, consisting of twice weekly supervised sessions; or
- Walking cohort, prompted remotely through a fitness tracker to achieve 150–300 active minutes per week.
Throughout this intervention period, and for a further 6 months following study conclusion, patients were assessed for changes in:
- Functional status
- Immune cell subsets
- Quality of life
Patient characteristics1
This study aimed to assess the feasibility of PA as an intervention; therefore, the patients selected were primarily fit or intermediate-fit and were classified as having non-active disease. Baseline characteristics are outlined in Table 1.
Table 1. Baseline characteristics*
|
ECOG, Eastern Cooperative Oncology Group performance status. |
|||
|
Characteristic, % (unless otherwise specified) |
Strength |
Walking |
p value |
|---|---|---|---|
|
Mean age (years) |
63.9 |
62.2 |
0.52 |
|
Mean body mass index (kg/m2) |
30.9 |
29.5 |
0.49 |
|
Sex |
|||
|
Female |
58.3 |
66.7 |
0.58 |
|
Male |
41.7 |
33.3 |
|
|
ECOG, baseline |
|||
|
0 fully active |
70.8 |
50 |
0.26 |
|
1 restricted in strenuous activity |
29.2 |
44.4 |
|
|
Disease status |
|||
|
Active disease |
4.2 |
16.7 |
0.17 |
|
Non-active disease |
95.8 |
83.3 |
|
|
Timepoints |
|||
|
Baseline |
100.0 |
94.4 |
0.36 |
|
3-month |
83.3 |
66.7 |
|
|
6-month |
79.2 |
66.7 |
|
|
3-months post-intervention |
75.0 |
61.1 |
|
|
6-months post-intervention |
79.2 |
61.1 |
|
Results
Functional status prior to and following the intervention period was determined using five assessments, outlined in Figure 1, to replicate the activities of daily living.
Figure 1. Assessments for functional status*
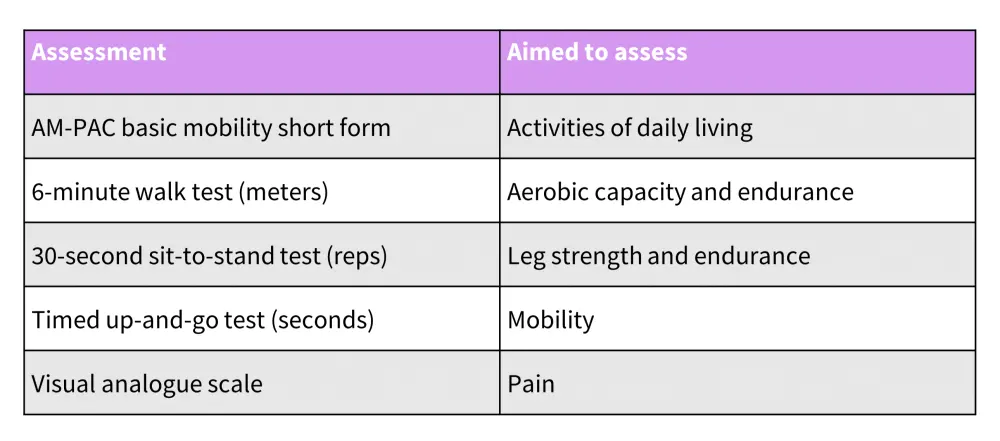
AM-PAC, activity measure for post-acute care.
*Adapted from Hillengass.1
In both cohorts, a significant improvement was observed in the activity measure for post-acute care (AM-PAC) form and the timed up-and-go test, with these results largely maintained at follow-up. However, in the sit-to-stand test, improvements observed over the trial period slowly decreased to baseline after the intervention ended.
T-cell exhaustion2
The ratio of exhausted to non-exhausted T-cells was lower at the end of the intervention period in all subsets. Changes in programmed cell death protein 1 and/or T-cell immunoreceptor with Ig and ITIM domain exhaustion markers are outlined in Table 3, with significant changes highlighted in bold.
Table 3. Ratio of exhausted to non-exhausted T cells*
|
PD-1, programmed cell death protein 1; TIGIT, T-cell immunoreceptor with Ig and ITIM domains. |
|||
|
Ratio, median |
Baseline |
Final |
p value |
|---|---|---|---|
|
CD4+ |
|||
|
PD-1+ or TIGIT+ |
1.33 |
1.15 |
0.14 |
|
PD-1+ |
1.18 |
0.92 |
0.17 |
|
TIGIT+ |
0.71 |
0.57 |
0.04 |
|
TIGIT+ and PD-1+ |
0.48 |
0.41 |
0.10 |
|
CD8+ |
|||
|
PD-1+ or TIGIT+ |
2.36 |
2.13 |
0.09 |
|
PD-1+ |
1.81 |
1.48 |
0.06 |
|
TIGIT+ |
1.91 |
1.67 |
0.18 |
|
TIGIT+ and PD-1+ |
1.25 |
1.01 |
0.17 |
Safety1
- There were no intervention-related Grade ≥3 adverse events.
- Adverse events were primarily musculoskeletal.
- There were no new fractures.
Conclusion
Physical activity in patients with MM is largely safe and had a positive impact on immunological and functional outcomes. There was also a benefit to quality of life and facilitation of patients returning to activities of daily living. A risk remains to patients in respect of musculoskeletal injury and potential subsequent impacts on frailty status. However, with trained supervision to maximize safety, PA offers a feasible intervention to improve the functional status of patients with MM.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?


