All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Supportive care in multiple myeloma: managing fatigue, cognitive impairment, and psychological wellbeing
Do you know... Which of the following is most likely to be a treatment-related rather than a disease-related symptom experienced by patients with multiple myeloma?
Multiple myeloma (MM) accounts for 10% of all hematologic malignancies.1 The overall survival (OS) of patients with MM has improved in recent years due to the availability of several therapies, such as monoclonal antibodies, cellular therapies, immunomodulators, and autologous stem cell transplantation. However, these therapies have related side effects, such as risk of anemia, bone lesions, hypercalcemia, infection, and renal failure, which causes fatigue, cognitive impairment, and depression. Despite improved treatment, MM is incurable and progressive, and often combined with durations of remission with minimal or maintenance therapy. Given the prospect of ongoing treatment-related complications, MM is associated with a significant decline in quality of life (QoL), highlighting the need for developing supportive care that addresses the long-term side effects of MM. Supportive care can help to improve QoL and maximize functional status as patients with MM live longer with the chronic burden of treatment-related complications.1
During the 48th Annual Meeting of the European Society for Blood and Marrow Transplantation (EBMT), Maaike de Ruijter1 presented on how patients with MM can be provided supportive care to improve their QoL. Here, we summarize an overview of the presentation, including the key supportive care measures for patients with MM.
Disease- and treatment-related symptoms
Patients with MM can experience either disease- or treatment-related symptoms (Figure 1), causing patients to be distressed. The National Comprehensive Cancer Network (NCCN) defines distress as “a multifactorial, unpleasant, emotional experience of a psychological, social and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment.”
Distress may cause patients to skip medication doses and reduce treatment efficacy, leading to poor treatment adherence, increased anxiety and depression, cause impaired cognitive function, and social isolation. Distress may make it difficult for patients to cope with cancer, and therefore, it is important to reassure patients that distress is normal during cancer. It is also essential to consider that distress symptoms may differ between patients and change over time; therefore, repeatedly asking patients about their symptoms is valuable. The NCCN Distress Thermometer and Problem List can be used to measure distress on a scale of 0 to 10.
Figure 1. Multiple myeloma disease- and treatment-related symptoms*
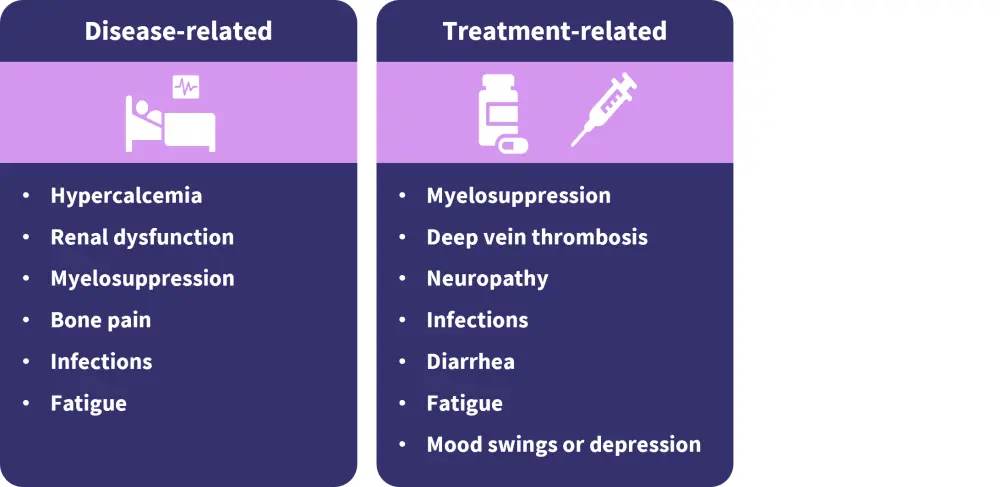
*Adapted from de Ruijter, et al.1
Fatigue
Fatigue is caused by pain, anemia, renal dysfunction, depression, and medication leading to reduced activity and insomnia in patients. The severity of fatigue will depend on the age of the patient and should be discussed with the patient, including offering tips on managing fatigue and screening tools.
Fatigue can be measured using the Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F) scale. This is a 40-item measure scale that assesses self-reported fatigue and its impact on daily activities and function. The FACIT-F scale includes the following domains and is available in several languages:
- Physical wellbeing
- Family wellbeing
- Emotional wellbeing
- Functional wellbeing
- Fatigue
A FACIT-F assessment should be followed by the following:
- Laboratory assessment for thyroid function and vitamin deficiency
- Physical assessment for cardiac function and pain
- Psychological assessment for depression, anxiety, and insomnia
- Drugs assessment
Patients experiencing fatigue should be offered stimulating exercises, physical therapy and dietician referral, and tips for improving sleep.
Depression/anxiety
The following indications should be observed in patients to check for signs of depression:
- Ongoing sad, hopeless, or empty mood
- Loss of interest or pleasure in activities once enjoyed
- Major weight loss/gain
- Changes in sleep
- Extreme tiredness
- Restless or slowed down
- Feelings of guilt, worthlessness, and helplessness
- Trouble focusing, remembering, and making decisions
- Thoughts of suicide or attempts at suicide
- Wide mood swings
Patients experiencing depression can be supported by lowering their dexamethasone/prednisolone dose, by understanding the difference between fatigue and depression, and by talking and listening to the patient and their caregivers or family.
Impaired cognitive functioning
The following indications should be observed in patients to check for signs of cognitive impairment:
- Issues with short-term memory
- Lack of concentration and poor recall
- Difficulty in multitasking
- Difficulty in reading books/watching movie
- Brain fog
The assessment of cognitive impairment should include checking for anemia, hypothyroidism, electrolyte imbalance, B12 deficiency, severe fatigue, sleeping problems, feelings of sadness or fear, and chemo brain due to chemotherapy.
The following scales can be used to measure cognitive functioning:
- Short test of mental status
- Montreal Cognitive Assessment (MoCA)
- Mini-Mental State Examination (MMSE)
- Clock-in-the-box test and 5-word delayed recall test
- Mini-Cog
Awareness amongst nurses of cognitive impairment in patients with MM is important. These patients may have difficulty remembering medication schedules or following multiple-step instructions and may not know what to do if they experience treatment-related side effects.
Medications for impaired cognitive function such as methylphenidate, amphetamine/dextroamphetamine, and memantine are not very effective and have side effects. Other treatment options are currently being investigated. Cognitive skills training may sometimes be helpful to the patients. It is important to talk to patients about cognitive impairment, measure it, identify the impact on family and caregivers, and assess if an intervention is needed. Mindfulness, a type of meditation that involves breathing methods, guided imagery, and other practices to relax the body and mind, may be a helpful option. Mindfulness may help to reduce feelings of anxiety and improve QoL and concentration.
Patients should be given the following advice to cope with impaired cognitive impairment:
- To do one thing at a time
- Take plenty of rest
- Do exercises to keep the brain active, such as swimming, walking, gardening, solving puzzles, word games, painting, and learning a new hobby
- Make notes and set reminders, or download a note-taking app
- Use a calendar to keep track of upcoming appointments, activities, and important dates
- Use sticky notes around the house and at work to remind of important tasks
SurvivorSHINE is a web-based lifestyle intervention for people living with cancer and is based on the American Cancer Society Diet and Physical Activity Guidelines and supported by evidence from three randomized controlled trials. SurvivorSHINE offers patients personalized information and tools to maintain a healthy weight through healthy eating and exercise.
Conclusion
This article provides an overview of how patients with MM can be supported to cope with fatigue, depression, and cognitive impairment. It highlights the importance of asking patients and their caregivers about the impact on QoL of the patient, reassuring patients that distress is common during cancer, repeatedly asking patients about their symptoms throughout the disease, and signposting patients and caregivers to help and support.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?




