All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Editorial theme | Incidence and diagnosis of AL amyloidosis
Amyloidosis refers to a rare and heterogeneous group of hematological disorders characterized by extracellular proliferation of proteins in tissues and organs to form insoluble fibrils, leading to organ failure. Increased levels of proteins due to an acquired or hereditary mutation, wild-type protein misfolding intrinsically, or transformation into amyloid form may contribute to amyloid formation. Deposition of amyloid forms may be local or systemic by affecting one or multiple organs, respectively. More than 30 proteins have been currently associated with amyloidosis, which can be localized, systemic, or either; different protein types define amyloidosis type.1
Amyloid light-chain (AL) amyloidosis is considered the most common subtype of amyloidosis, characterized by elevated levels of free light chains (FLCs).1 There are significant challenges in its diagnosis and management, one of which being that no treatment is currently approved. A number of therapeutic approaches, including daratumumab plus cyclophosphamide, bortezomib, and dexamethasone (CyBorD), bendamustine plus dexamethasone, and ixazomib plus dexamethasone, are under evaluation for the treatment of systematic AL amyloidosis, demonstrating promising results.
Throughout this new editorial theme, we will review AL amyloidosis diagnosis, prognosis, and treatment. This first article will focus on the incidence and diagnosis, to raise awareness of this rare disease. Stay tuned for future updates!
Incidence
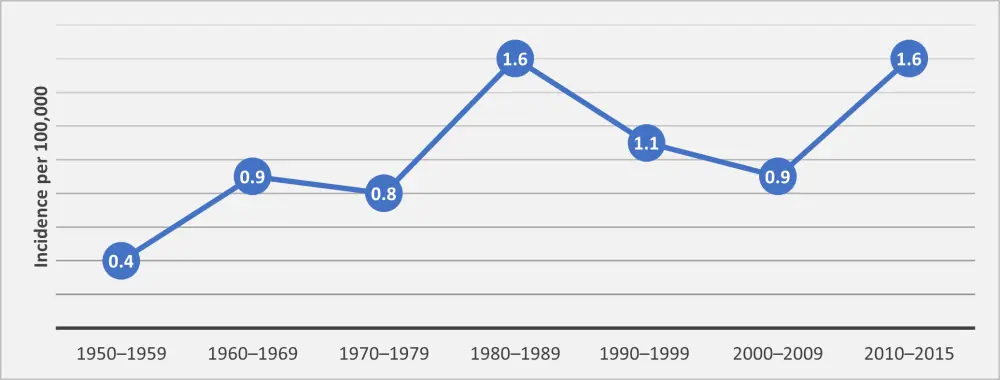
In the United States, the incidence of AL amyloidosis is expected to be around 3,800 cases per year, with a median age of 76 years at the time of diagnosis. Based on a study conducted by Robert A. Kyle et al.,2 age- and sex-adjusted incidence rate between 1990 and 2015 was estimated to be 1.2/100,000 person-years. The incidence rates were comparable when estimated by decades. Annual incidence rates between 1950 and 2015 are shown in Figure 1.
Figure 1. Adjusted incidence rates of AL amyloidosis in the US by decade2
In Europe, between 1999 and 2018, the number of patients diagnosed with AL amyloidosis was 29,777, leading to a 20-year diagnosed prevalence of 58.09 per million. The prevalence ranged between 42.99 (Cyprus) to 65.38 (Italy) per million among European Medicines Agency (EMA) member states. The incidence was estimated to be 11.74 per million (range, 8.94 for Cyprus to 13.29 for Italy) in 2018.3
Diagnosis
The diagnosis of AL amyloidosis can be challenging as there is no single test to identify this disorder, and symptoms can be similar to those seen in more prevalent diseases. Events that may be suggestive of AL amyloidosis include the following4:
- Nephrotic syndrome not related to diabetes
- Nonischemic cardiomyopathy along with hypertrophy
- Hepatomegaly or elevated alkaline phosphatase levels without abnormalities of liver
- Chronic inflammatory demyelinating polyneuropathy with a monoclonal protein
- Monoclonal gammopathy with unexplained fatigue, edema, weight loss, or parethesia
Some of these events may develop in smoldering multiple myeloma (SMM) and monoclonal gammopathy of undetermined significance (MGUS); however, routine amyloid staining of the bone marrow is not considered typical for MGUS or SMM and, therefore, should raise suspicion for amyloidosis.4
Angela Dispenzieri gave a talk on the diagnosis of amyloidosis during the XVII International Society of Amyloidosis (ISA) Symposium.5 She stated that medical consultation by experts of different fields—including cardiology, nephrology, hematology—and incidental findings on imaging with an echocardiogram, computed tomography (CT) of body, magnetic resonance imaging (MRI) of the heart, and laboratory evaluation could guide diagnosis. If there is an incidental finding on tissue biopsy, amyloid typing can be considered. The algorithm for diagnosis is depicted in Figure 2.
Figure 2. Diagnostic algorithm for amyloidosis (adapted from Dispenzieri5)
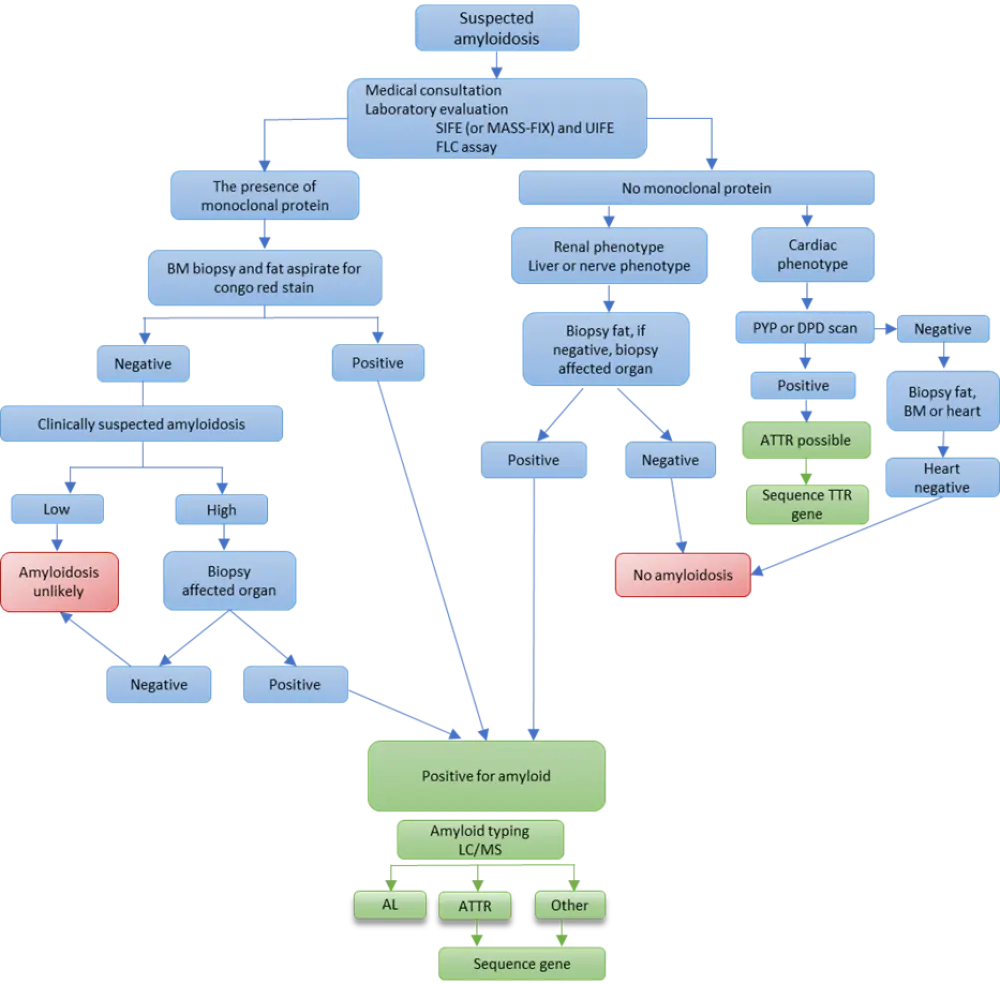
Amyloid typing is considered critical for a correct diagnosis and disease classification. It can be done by immunochemistry, immunofluorescence, immunoelectron microscopy, or laser dissection/liquid chromatography plus tandem mass spectrometry. Among these methods, laser dissection/liquid chromatography plus tandem mass spectrometry is deemed to be the gold standard in typing.5 Relevant tests for amyloidosis diagnosis and monitoring are shown in Table 1.
Table 1. AL amyloidosis tests5
|
EKG, electrocardiogram; FLC, free light chain; MASS-FIX, mass-spectrometry fixation; MRI, magnetic resonance imaging; SPEP, serum protein electrophoresis. |
|
|
Tissue biopsy |
Congo red stain; type amyloid protein |
|
Blood tests |
Alkaline phosphatase, bilirubin, creatinine, albumin, uric acid, factor X |
|
|
Troponin, N-terminal brain natriuretic peptide |
|
|
Immunoglobulin FLC, SPEP with immunofixation (or MASS-FIX) |
|
24-hour urine |
Protein electrophoresis with immunofixation |
|
Cardiac evaluation |
EKG, cardiac imaging |
|
As clinically indicated |
Diagnostic imaging of liver and spleen |
|
|
Fecal fat measurements |
|
|
Serum carotene levels |
|
|
Nerve conduction studies |
|
|
Serum amyloid P scan |
|
|
Heart MRI to eliminate cardiac involvement |
|
|
Holter monitoring |
The importance of early diagnosis in amyloidosis6
During the XVII International Symposium on Amyloidosis, Ute Hegenbart provided insight on the warning signs to look out for to get an early diagnosis, as most patients are diagnosed at a late stage.6 It is considered crucial to diagnose patients at an early stage to improve overall survival, quality of life, maintain organ function, and be eligible for more treatment options.
As a sign, in some patients, NT-proBNP has been shown to indicate cardiac involvement before cardiac failure symptoms appear. Cardiac MRI is also beneficial in cases where a normal electrocardiogram is obtained, and NT-proBNP values can be used to detect cardiac involvement. These signs may raise the alarm in patients already diagnosed with clonal B cell disorders and elevated FLC, including MGUS, SMM, symptomatic MM, or secretory B cell non-Hodgkin lymphoma. In these patients, regular intensive anamnesis, clinical examination, NT-proBNP and albuminuria evaluation, or congo red staining on bone marrow and other routine biopsies may be beneficial for early diagnosis. If amyloidosis is suspected, fat aspiration should also be performed.
Conclusion
Currently, there is a hazardous delayed diagnosis of patients with AL amyloidosis, which has a high impact on their overall status and the possibility of treating them with more aggressive therapies, which ultimately leads to shorter survival. Of note, this is a multidisciplinary disease and, as such, it can be detected first by other clinical specialties. To conclude, there is a need to raise awareness of AL amyloidosis, particularly among hematologists, as they play a crucial role in early diagnosis.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?

