All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
The impact of second primary and second hematological malignancies on survival outcomes of MM after auto-HSCT
The recent developments in the treatment of multiple myeloma (MM) have led to improved overall survival (OS) rate among patients. However, emerging clinical data on lenalidomide-maintained MM post-autologous hematopoietic stem cell transplantation (auto-HSCT) have revealed an increased rate of secondary primary malignancies (SPM) and secondary hematological malignancies (SHM).
Ragon and colleagues recently published a retrospective cohort analysis in Blood Advances on the incidence and clinical impact of SPM in patients with MM who underwent auto-HSCT with melphalan conditioning. The Multiple Myeloma Hub is pleased to summarize the analysis here.
Study design and baseline characteristics1
This was a large retrospective cohort analysis of adult patients with MM who underwent first auto-HSCT with melphalan conditioning between 2011 and 2018 in the USA. Data on eligible patients were collected from the Center for International Blood and Marrow Transplant Research database.
The primary objective was to assess the impact of SPM and SHM on OS and progression-free survival (PFS). The secondary objective was to characterize different types of SPM after auto-HSCT. Selected baseline characteristics are shown in Table 1.
Table 1. Patient characteristics*
|
HSCT-CI, hematopoietic stem cell transplantation comorbidity index; HR, high risk; HSCT, hematopoietic stem cell transplant; Ig, immunoglobulin; ISS, International Staging System. *Adapted from Ragon, et al.1 |
|
|
Characteristic %, unless otherwise specified |
Total cohort |
|---|---|
|
Median age at first auto-HSCT, years (range) |
61 (20–82) |
|
Sex, male |
55 |
|
Race |
|
|
White |
58 |
|
Black or African American |
34 |
|
Other |
5 |
|
Karnofsky score |
|
|
≥90 |
53 |
|
<90 |
46 |
|
HSCT-CI |
|
|
0 |
26 |
|
1–2 |
31 |
|
3–5 |
35 |
|
6+ |
7 |
|
Prior malignancy |
|
|
No |
90 |
|
Yes |
10 |
|
ISS stage at diagnosis |
|
| I |
31 |
|
II |
28 |
|
III |
18 |
|
Immunochemical subtype |
|
|
IgG |
60 |
|
IgA |
19 |
|
Light chain |
19 |
|
Non-secretory |
1 |
|
Cytogenetics |
|
|
Standard risk |
63 |
|
High risk |
28 |
|
t(4;14) |
3 |
|
t(14;16) |
1 |
|
del17p |
4 |
|
+1q |
14 |
|
≥2 HR |
6 |
|
Lines of chemotherapy |
|
|
1 |
72 |
|
2 |
24 |
Results1
Incidence of SPM and SHM
At a median follow up of 37 months:
- SPMs were identified in 4% of the patients.
- Among these, solid tumors accounted for 64%, with a median time to development of 33 months (range, 2–96 months)
- SHMs accounted for 36% with a median time to development of 35 months (range, 3–93 months)
- The most common types of SPMs included melanoma and genitourinary malignancies occurring in 19% and 18% of patients, respectively.
- For the entire cohort, the cumulative incidences of SPM and SHMs at 3 years were 3.3% and 1.1%, respectively
The incidence and classification of SPMs is shown in Figure 1.
Figure 1. A. Incidence of SPMs in total cohort and B. Classification of SPMs*
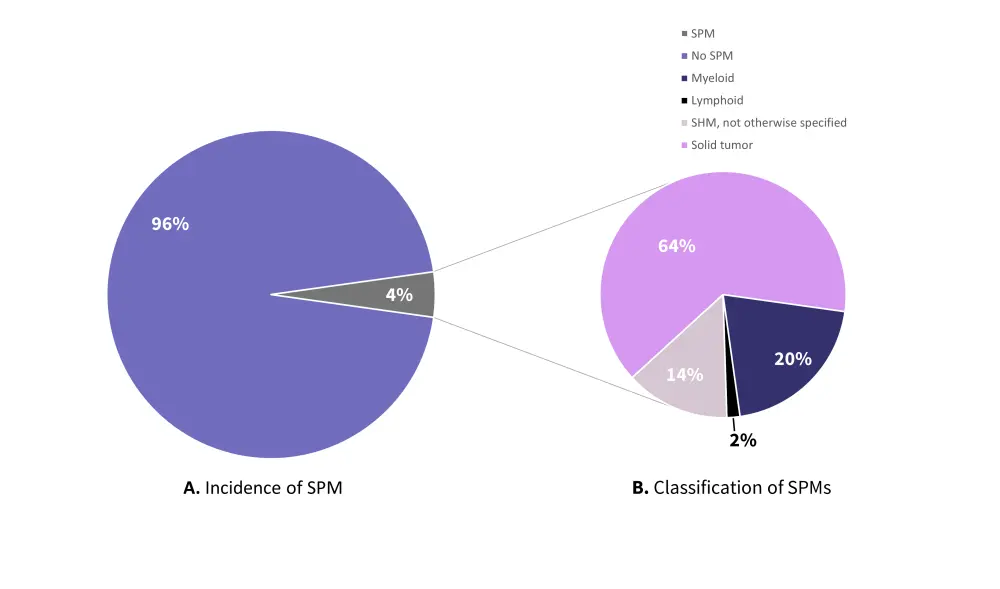
SHM, secondary hematological malignancy; SPM, secondary primary malignancy.
*Data from Ragon, et al.1
Mortality rates
- Amongst the 96% of patients who did not develop a SPM, 16% of patients died at the final follow-up compared with 38% in the SPM cohort.
- MM was the primary cause of death, responsible for 85% and 42% of deaths in both the no SPM and SPM cohorts, respectively.
- SPM was responsible for 30% of deaths in the SPM cohort.
Clinical outcomes
- PFS rates were inferior in the SPM vs no SPM population (hazard ratio [HR], 2.62; 95% confidence interval [CI], 2.03–3.38; p < 0.001)
- In the SHM subgroup, PFS rates were even poorer (HR, 5.01; 95% CI 3.41–7.37; p < 0.001)
- OS rates were also inferior in the SPM vs no SPM population (HR, 3.85; 95% CI, 2.95–5.02; p < 0.001)
- In patients with SPM, presence of SHM resulted in significantly poorer OS rates (HR, 8.13; 95%CI, 5.67–11.65; p < 0.001)
- Other factors associated with poorer PFS in the SPM population included:
- Male sex (p = 0.0742); higher ISS stage at diagnosis (p < 0.0001); high-risk cytogenetics (p < 0.0001); low Karnofsky performance status (p = 0.0939); and ≥2 lines of therapy pre-transplant (p < 0.0001).
- Similarly, factors associated with poorer OS in the SPM population included:
- Male sex (p = 0.2683); higher ISS stage at diagnosis (p < 0.0001); high-risk cytogenetics (p < 0.0001); low karnofsky performance status (p = 0.0021); and ≥2 lines of therapy pre-transplant (p < 0.0001).
Conclusion
This cohort analysis showed that the presence of SPM post auto-HSCT is associated with inferior clinical outcomes and survival in patients with MM, particularly for patients with SHM. However, when considering the data from this retrospective analysis it is important to consider certain limitations such as accuracy of reporting, availability of data on duration of maintenance therapy, post-HSCT treatment and therapies for SPM, which may have influenced the incidence or impact of SPM or SHM. For instance, 10% of patients had a second malignancy prior to auto-HSCT which arguably means recurrence cannot be classified as a SPM. This analysis highlights the patients with post auto-HSCT SPMs as a key group for further research.
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?



