All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
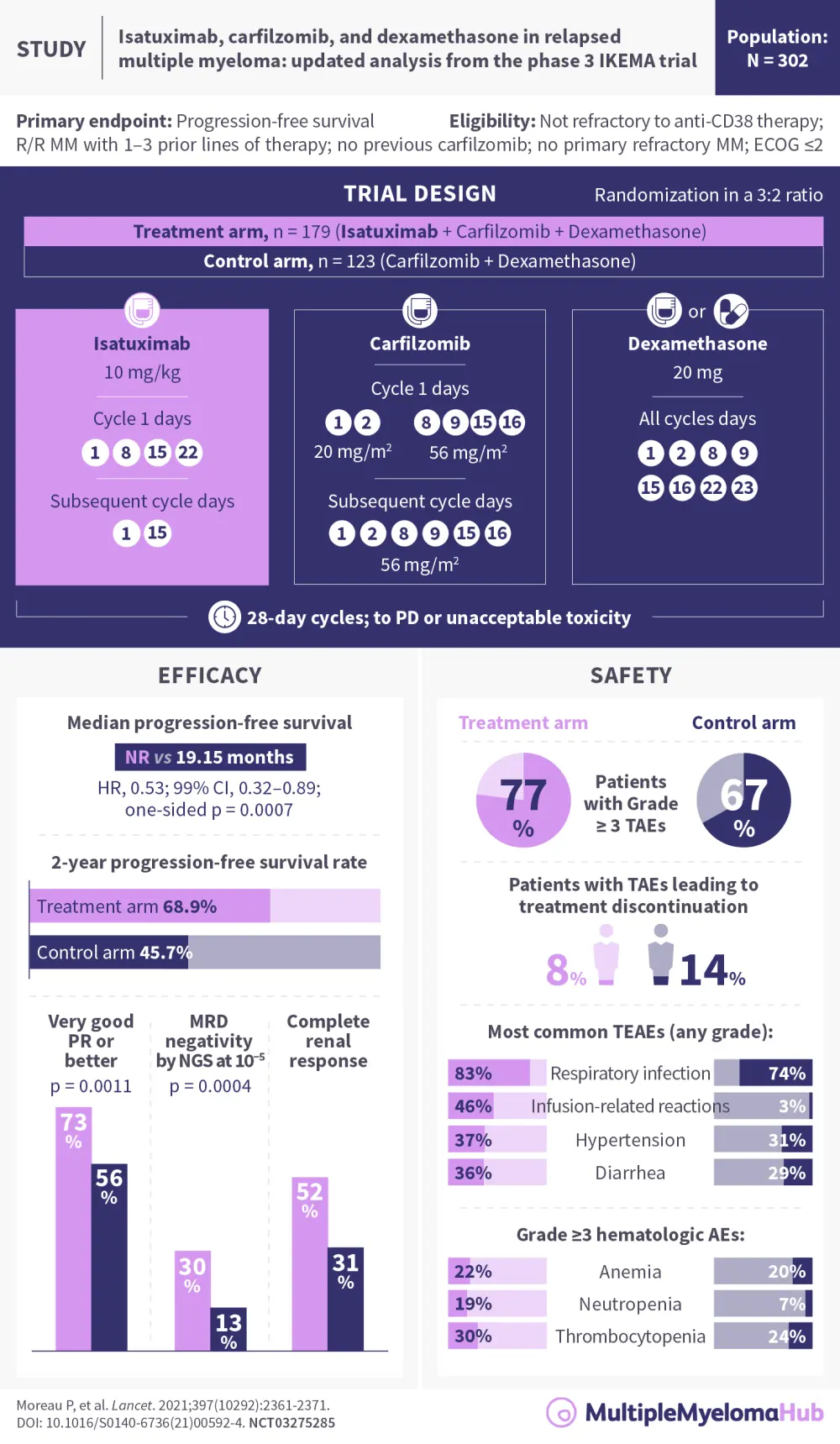
IKEMA: Isatuximab in combination with the standard-of-care regimen carfilzomib + dexamethasone for the treatment of R/R multiple myeloma
Visual abstract
In March 2021, the U.S. Food and Drug Administration (FDA) approved isatuximab in combination with carfilzomib and dexamethasone for the treatment of relapsed/refractory multiple myeloma (MM) in patients who had received one to three prior lines of therapy.1 The FDA approval for this indication was followed, in April 2021, by European Commission (EC) approval, representing a new treatment option for patients with MM who are refractory to lenalidomide.2 Both the FDA and EC approvals were previously reported on the Multiple Myeloma Hub, as were the results of the trial upon which these approvals were based.
An updated analysis of the IKEMA trial, summarized in the above visual abstract, was published in Lancet in June 2021, and several subgroup analyses were presented by Ivan Spicka and colleagues at the 2021 American Society for Clinical Oncology (ASCO) Annual Meeting. Here we present key results from the subgroup analyses.
Progression-free survival in key subgroups
In the prespecified subgroup analyses, isatuximab with carfilzomib-dexamethasone (Isa-Kd) demonstrated greater clinical benefit across almost all subgroups.3 Isa-Kd provided a consistent benefit vs Kd in elderly patients. In total, 52 patients ≥70 years were treated with isatuximab and achieved a longer progression-free survival (PFS) than the control group (n = 34) (hazard ratio, 0.36; 95% confidence interval, 0.176–0.751). Within the experimental arm, complete response and very good partial response or better (≥VGPR) rates were similar between younger and older patients. Fewer old patients discontinued the study treatment due to treatment-emergent adverse events in the triplet arm (11.8% vs 23.5%).
Regarding high-risk MM, defined as presence of t(4;14), del(17p), and t(14;16)] and/or gain(1q21), responses were similar for high-risk patients, but depth of response improved considerably with isatuximab in patients with gain or amplification of 1q21 (≥VGPR rates, 73.3% vs 51.9% and 65.6% vs 40%, respectively).4
There was a PFS benefit trend towards Isa-Kd in patients harboring at least one of the chromosomal abnormalities studied (hazard ratio, 0.724; 95% confidence interval, 0.361–1.451). Patients with high-risk cytogenetics or gain(1q21) experienced a higher rate of Grade ≥3 treatment-emergent adverse events with Isa-Kd (85.7% and 80.8%, respectively) vs the control arm and vs the standard risk subgroup, but it did not impact the number of patients discontinuing the study treatment (4.8% and 6.8%, respectively).
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?

