All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Factors associated with unsustained MRD-negativity in patients with MM eligible for transplant
Measurable residual disease (MRD) negativity is increasingly being investigated and used as a biomarker for treatment cessation in patients with multiple myeloma (MM) who are eligible for transplant.
However, MRD resurgence and progressive disease (PD) are observed in some patients posttreatment cessation guided by MRD-negativity; highlighting the importance of identifying risk factors and predictors of resurgence in this population to prevent disease progression.
Here, we summarize a report published by Guerrero et al.1 in Blood on the predictors of unsustained MRD-negativity in patients with MM who are eligible for transplant.
Patient population1
- Individuals enrolled in the GEM2012MENOS65 (NCT01916252) and GEM2014MAIN (NCT02406144) trials who had reached MRD-negativity, as measured by next generation flow were included in this study (N = 267)
- Of these patients, initial MRD-negativity was reached:
- After induction; 46.8%
- High-dose therapy/autologous stem cell transplantation; 28.8%
- Consolidation; 12.0%
- After 1-year of maintenance; 12.4%
- Median time to initial MRD-negativity was 9 months
- Median follow-up after first MRD-negativity was 73 months
- Patients were evaluated for MRD resurgence and PD, using next generation flow and stratified by characteristic
Key findings1
- At follow-up, MRD resurgence or PD was observed in 42% of patients
- 4% of patients died without PD
- Factors associated with increased MRD-resurgence/PD risk were International Staging System (ISS) score of 3, and ≥0.01% circulating tumor cells (Figure 1).
- Late occurring MRD negativity; defined as MRD-negativity achieved later than post-induction, was also associated with increased resurgence/PD.
- 5-year MRD resurgence and/or PD rates (P < 0.001):
- 0 risk factors; 16%
- 1 risk factor; 33%
- ≥2 risk factors; 57%
- Approximately 15% of patients relapsed without previously observed MRD resurgence
- 72% of these patients had not received MRD assessment within the last year
- Median PFS from MRD resurgence until either PD or death was 39 months.
- Of patients who relapsed vs those who were progression-free after MRD resurgence, rates of ISS 2 and 3 were significantly higher than ISS 1 at 75% and 46%, respectively (p = 0.03).
Figure 1. Hazard ratio for predictors of MRD-resurgence and PD*
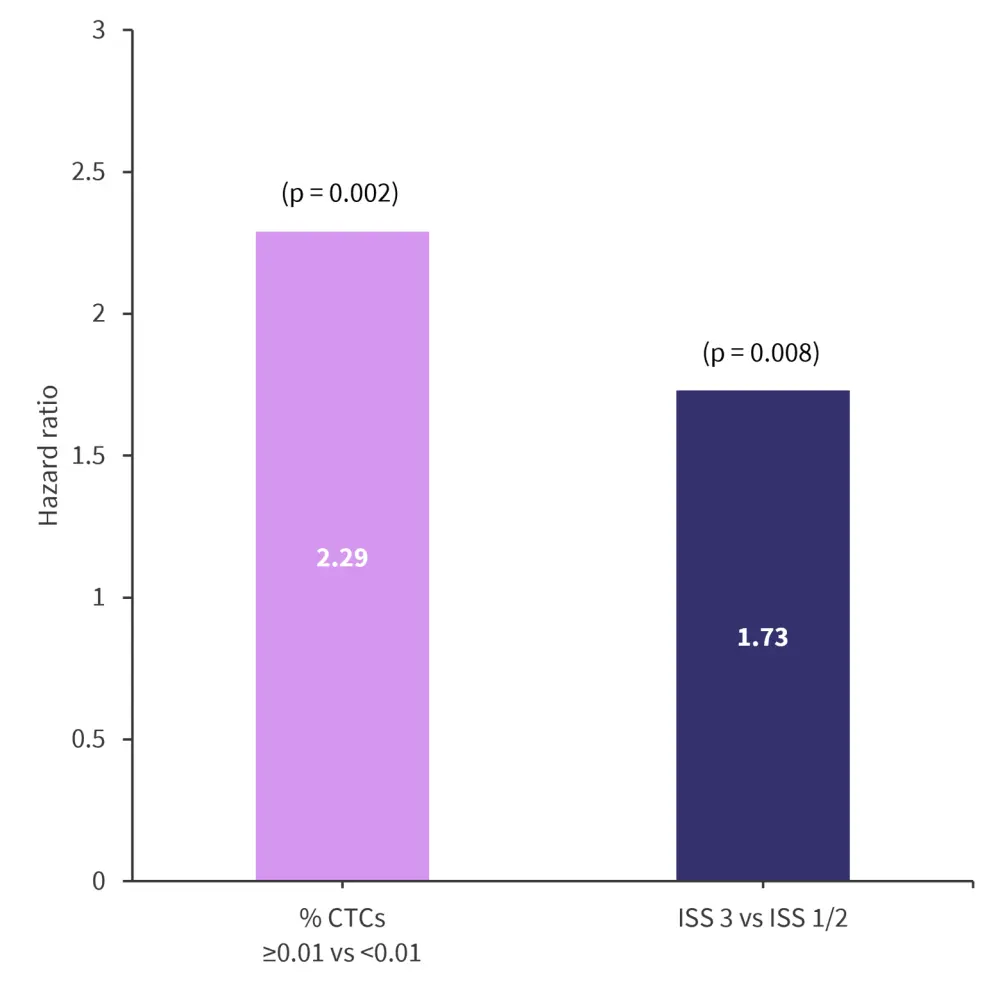
CTC, circulating tumor cells; ISS, International Staging System.
*Adapted from Guerrero, et al.1
|
Key learnings |
|---|
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?



