All content on this site is intended for healthcare professionals only. By acknowledging this message and accessing the information on this website you are confirming that you are a Healthcare Professional. If you are a patient or carer, please visit the International Myeloma Foundation or HealthTree for Multiple Myeloma.
The mm Hub website uses a third-party service provided by Google that dynamically translates web content. Translations are machine generated, so may not be an exact or complete translation, and the mm Hub cannot guarantee the accuracy of translated content. The mm and its employees will not be liable for any direct, indirect, or consequential damages (even if foreseeable) resulting from use of the Google Translate feature. For further support with Google Translate, visit Google Translate Help.
The Multiple Myeloma Hub is an independent medical education platform, sponsored by Bristol Myers Squibb, GSK, Legend Biotech, Pfizer, and Roche. Funders are allowed no direct influence on our content. The levels of sponsorship listed are reflective of the amount of funding given. View funders.
Now you can support HCPs in making informed decisions for their patients
Your contribution helps us continuously deliver expertly curated content to HCPs worldwide. You will also have the opportunity to make a content suggestion for consideration and receive updates on the impact contributions are making to our content.
Find out more
Create an account and access these new features:
Bookmark content to read later
Select your specific areas of interest
View multiple myeloma content recommended for you
Auto-HCT in newly diagnosed MM with del(17p): real-world outcomes
The median survival for patients with multiple myeloma (MM) has surpassed 10 years following the introduction of novel therapies, such as immunomodulatory drugs, proteasome inhibitors, and anti-CD38 monoclonal antibodies. However, deletion of the short arm of chromosome 17 (17p13.1; del[17p]) remains one of the most powerful predictors of poor outcomes.
During the 50th Annual Meeting of the European Society for Blood and Marrow Transplantation (EBMT), Marcoux et al. presented a real-world study investigating outcomes with upfront autologous hematopoietic stem cell transplantation (auto-HCT) in newly diagnosed MM (NDMM) with del(17p).1 Here, we summarize the key findings.
Methods1
- This was a single-center retrospective study conducted in patients with NDMM and del(17p) receiving upfront auto-HCT between 2008 and 2018.
- The primary endpoints were progression-free survival (PFS) and overall survival (OS).
- Secondary endpoints were hematologic response and measurable residual disease (MRD) status posttransplantation.
Key findings1
- Overall, 115 patients with del(17p) were included.
- Median age at auto-HCT was 62 years and 55% were male.
- Post-induction therapy, 29% of patients achieved an MRD negative ≥very good partial response (VGPR) prior to auto-HCT. This improved to 55% at Day 100 post-auto-HCT and at best auto-HCT response (Figure 1.)
Figure 1. Key real-world outcomes with auto-HCT in NDMM with del(17p)*
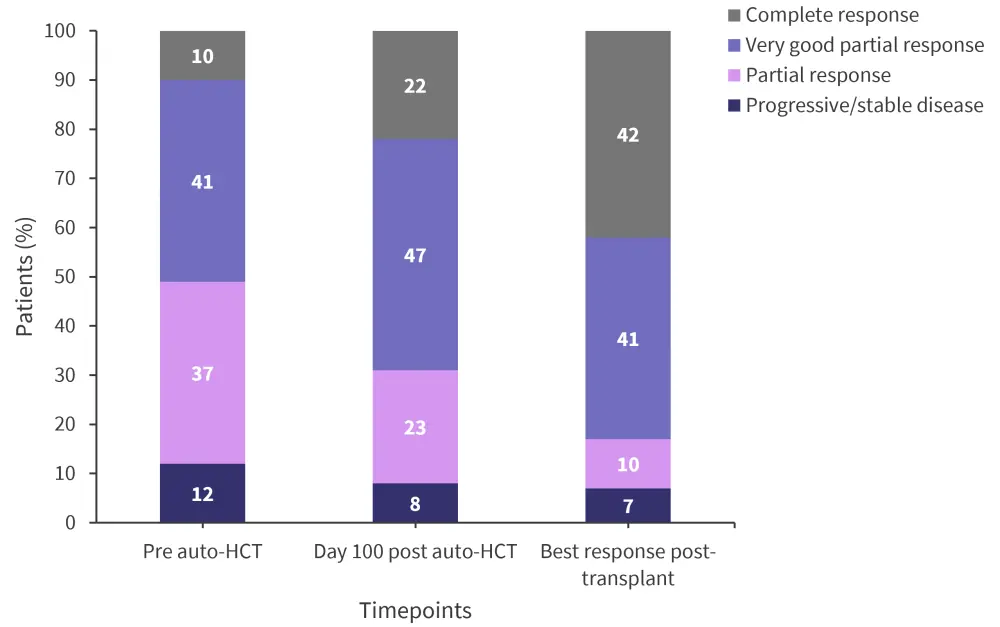
Auto-HCT, autologous hematopoietic stem cell transplantation.
*Adapted from Marcoux, et al.1
- At a median follow-up of 31.4 months, median PFS for the entire cohort was 19.9 and OS was 71.5 months; 5-year PFS and OS were 32% and 53%, respectively.
- Patients with both t(4;14) and del(17p) had poor outcomes, with a median PFS of 11.5 months and OS of 22.4 months. However, patients achieving MRD negative ≥VGPR prior to auto-HCT had a median PFS of 71.9 months and OS of 92.4 months.
- In multivariable analysis, female sex was significantly associated with worse PFS, while MRD negativity and maintenance therapy were significantly associated with improved PFS post auto-HCT (Figure 2).
- Regarding OS, female sex and presence of t(4;14) were significantly associated with worse OS, while Karnofsky performance status of ≥90 was significantly associated with improved OS.
Figure 2. Multivariate analysis for A progression free survival and B overall survival*
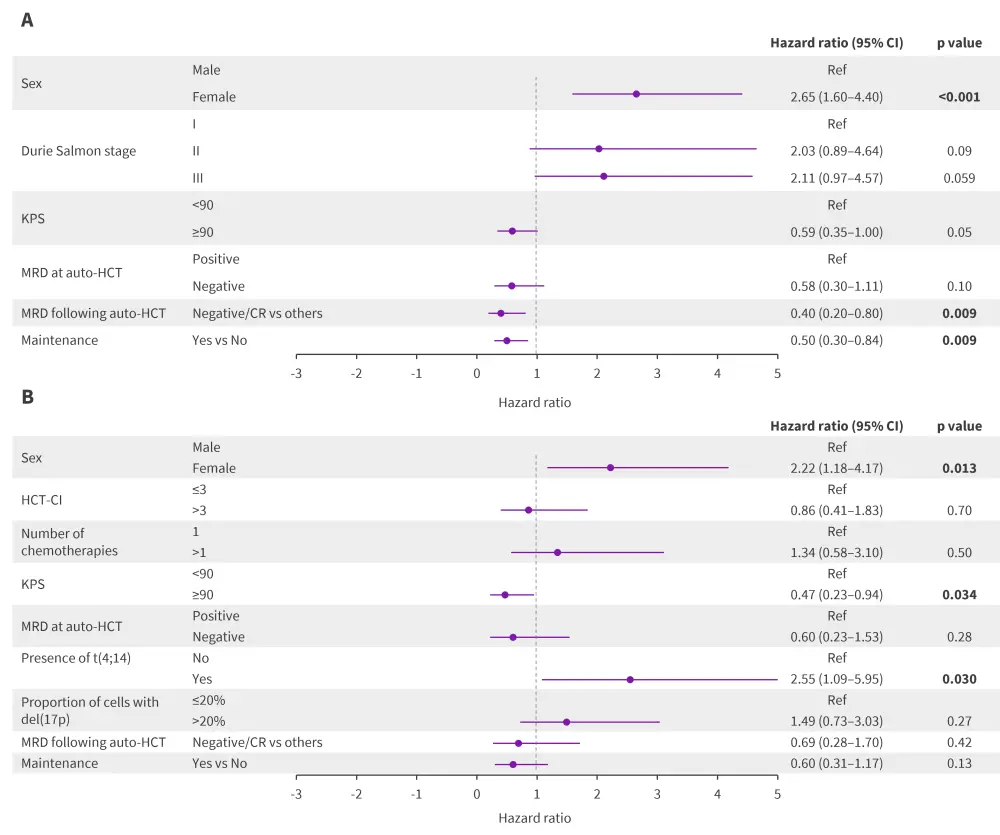
Auto-HCT, autologous hematopoietic stem cell transplantation; CI, confidence interval; CR, complete response; HCT-CI, Hematopoietic Cell Transplantation-specific Comorbidity Index; KPS, Karnofsky performance status; MRD, minimal residual disease.
*Data from Marcoux, et al.1
|
Key learnings |
|---|
|
References
Please indicate your level of agreement with the following statements:
The content was clear and easy to understand
The content addressed the learning objectives
The content was relevant to my practice
I will change my clinical practice as a result of this content
Your opinion matters
On average, how many patients with MGUS/smoldering MM do you see in a month?

